When someone struggles to breathe, it’s easy to assume it’s asthma. But what if it’s not? Asthma and COPD look similar on the surface-both cause wheezing, coughing, and shortness of breath. Yet they’re fundamentally different diseases with different causes, progression paths, and treatments. Getting the diagnosis wrong can mean the difference between managing symptoms effectively and watching your lung function decline without stopping.
What’s Really Going On in the Lungs?
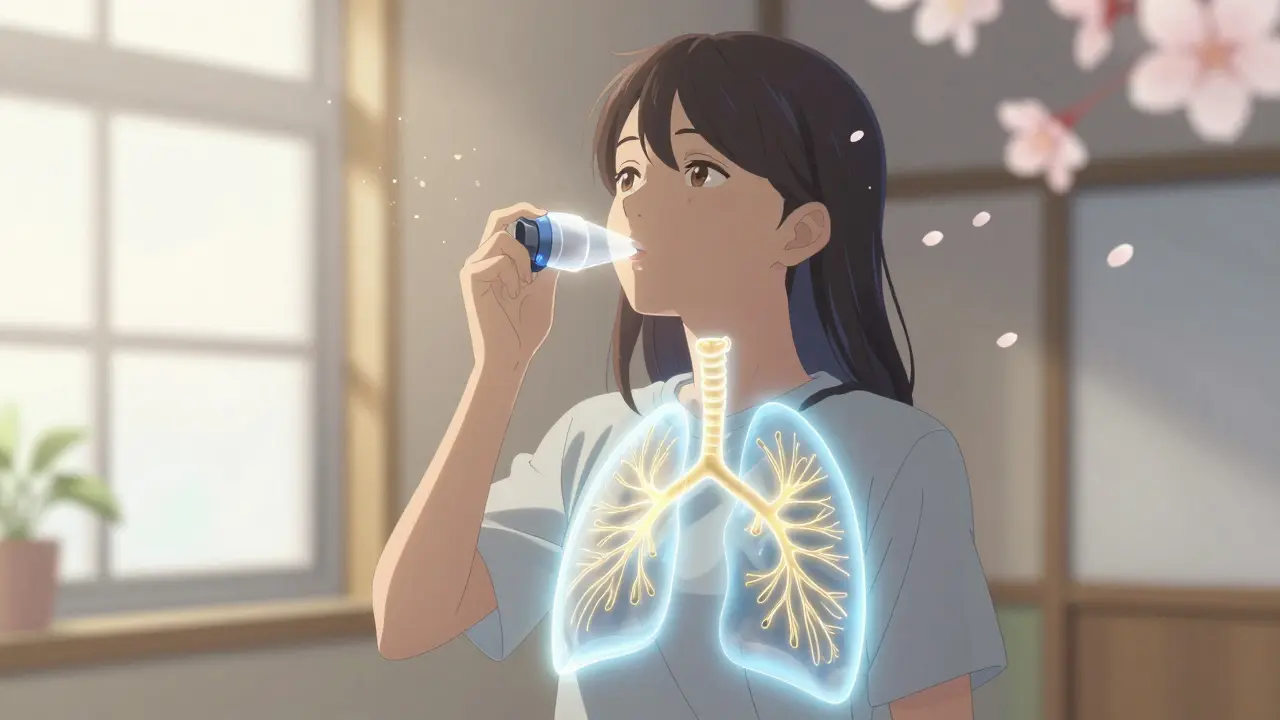
Asthma is an inflammatory condition where the airways become overly sensitive and react strongly to triggers like pollen, cold air, or exercise. When this happens, the muscles around the airways tighten, the lining swells, and mucus builds up. The good news? This narrowing is usually reversible. After using an inhaler or even just resting, most people with asthma can breathe normally again. That’s why many asthma patients go weeks or even months without symptoms.
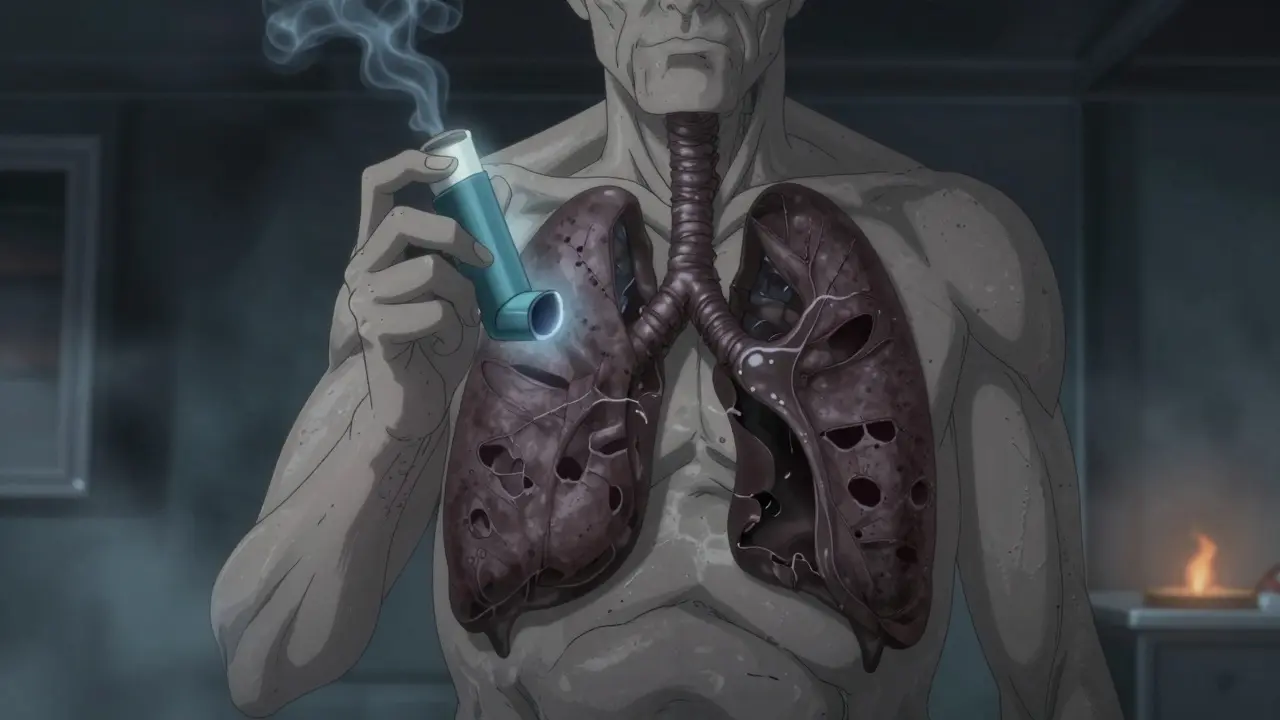
COPD, on the other hand, is damage. It’s not just inflammation-it’s destruction. Most cases come from long-term smoking, which breaks down the air sacs in the lungs (emphysema) and thickens the airway lining with mucus (chronic bronchitis). This damage doesn’t heal. Once lung tissue is gone, it’s gone. Airflow gets stuck, and breathing becomes harder with every passing year. Unlike asthma, COPD symptoms don’t disappear between flare-ups. They just get worse.
Symptoms: When It’s Not Just a Bad Day
Both conditions cause coughing and breathlessness, but the patterns tell the story.
- Asthma: Symptoms often come and go. Nighttime coughing, wheezing after exercise, or tightness in the chest after exposure to allergens are classic signs. Many asthma patients describe their cough as dry-little to no phlegm. About 68% of asthma sufferers have symptom-free periods between attacks.
- COPD: Symptoms are constant. A daily cough that produces thick mucus (87% of cases), ongoing shortness of breath even at rest, and fatigue that won’t go away are hallmarks. People with advanced COPD often develop cyanosis-a bluish tint around the lips or fingernails-because their blood isn’t getting enough oxygen. Only 12% of COPD patients report any real break from symptoms.
Age matters too. Asthma often starts before age 10. Eighty percent of cases are diagnosed before age 30. COPD? Almost never. Over 90% of COPD diagnoses happen after age 45. If someone over 50 starts having breathing problems and has a history of smoking, COPD is far more likely than asthma.
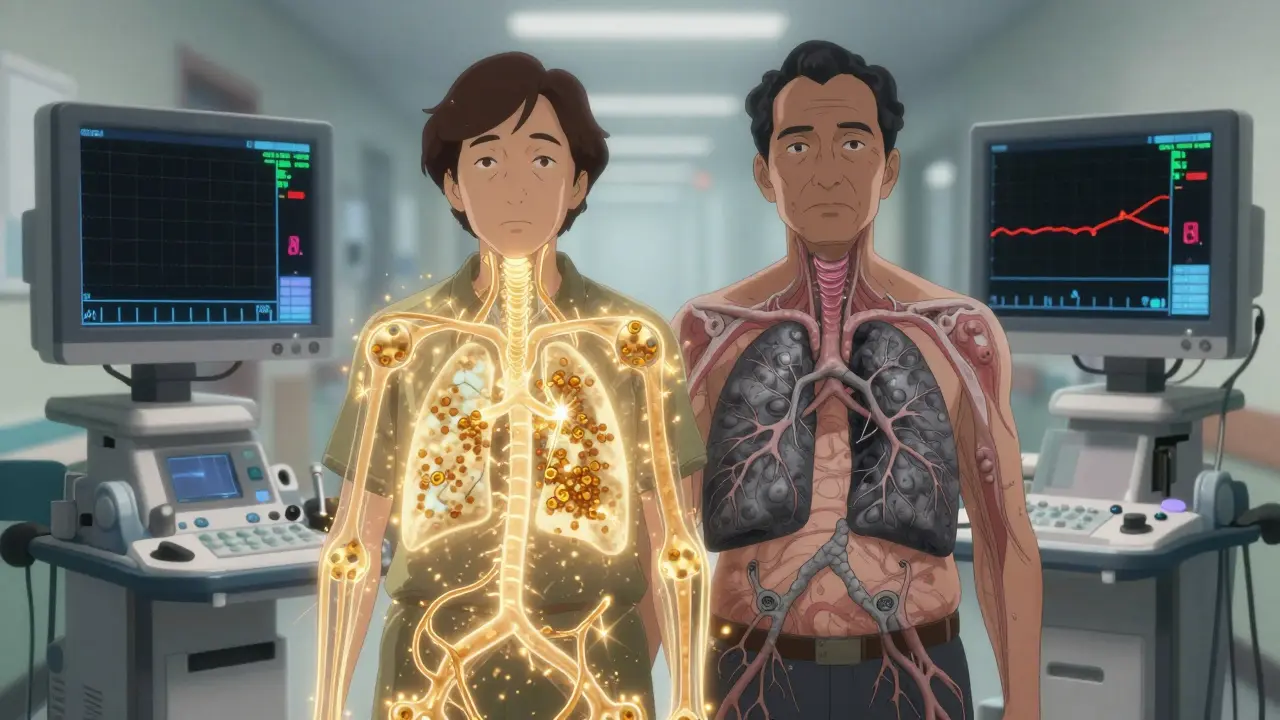
How Doctors Tell Them Apart
It’s not just about symptoms. Doctors use tests to see what’s really happening inside the lungs.
One key test is spirometry. It measures how much air you can blow out and how fast. In asthma, after using a bronchodilator (a puff that opens airways), lung function usually improves by 12% or more. That’s reversibility in action. In fact, 95% of asthma patients show this kind of improvement.
In COPD? Not so much. Only about 15% of COPD patients show that level of improvement. Their airflow limitation is mostly fixed. That’s why doctors look for other clues.
FeNO testing-measuring nitric oxide in your breath-helps too. High levels (above 50 ppb) suggest eosinophilic inflammation, which is typical in asthma. COPD patients usually have levels below 25 ppb. Blood tests for eosinophils (a type of white blood cell) add another layer: counts above 300 cells/μL point toward asthma or overlap, while counts below 100 suggest pure COPD.
CT scans show even more. In 75% of COPD patients, you’ll see emphysema-holes in the lung tissue. In asthma? Only 5% show that. Allergies are another clue. Sixty-five percent of asthma patients have hay fever. Only 22% of COPD patients do.
Treatment: One Size Does Not Fit Both
Asthma treatment is about controlling inflammation and preventing attacks. First-line treatment? Short-acting inhalers like albuterol for quick relief. If symptoms are frequent, daily inhaled corticosteroids (ICS) are added to calm the airway inflammation. For the 5-10% with severe, allergy-driven asthma, biologics like omalizumab or mepolizumab target specific immune pathways. The goal? Near-zero symptoms. Eighty-nine percent of asthma patients can achieve good control with proper treatment.
COPD treatment is about keeping airways open and slowing decline. Bronchodilators come first-long-acting ones (LABAs and LAMAs). These don’t cure anything, but they help you breathe easier day to day. Inhaled steroids (ICS) are only added if you’re having frequent flare-ups. Why? Because steroids don’t fix the underlying damage, and they come with side effects like increased risk of pneumonia. Pulmonary rehab is critical: it helps COPD patients walk farther and feel less winded. On average, they gain 54 meters in a 6-minute walk test after rehab.
Here’s the hard truth: only 52% of COPD patients report satisfactory symptom control. That’s because the damage is permanent. You can slow it, but you can’t undo it.
The Overlap: When It’s Neither-Or Both
Between 15% and 25% of people with obstructive lung disease have something called Asthma-COPD Overlap Syndrome (ACOS). These patients have features of both: they may have eosinophilic inflammation like asthma, but also fixed airflow blockage like COPD.
ACOS patients often have worse outcomes. They’re hospitalized more often, need emergency care more frequently, and struggle more with daily activities. A 2022 survey found that 78% of specialists treat ACOS with triple therapy-two long-acting bronchodilators plus an inhaled steroid. But evidence for this approach is still limited. The challenge? It’s hard to know if you’re treating asthma, COPD, or both.
Prognosis: What to Expect Down the Road
Long-term outlooks differ sharply. Someone with moderate asthma has a 92% chance of surviving 10 years. Someone with moderate COPD? About 78%. Smoking changes everything. In COPD, quitting smoking cuts disease progression by 50%. In asthma, smoking doesn’t change much-unless it’s pushed the condition into ACOS.
And here’s something surprising: 15-20% of people who’ve had asthma for over 20 years develop fixed airflow limitation. That means their asthma starts to look more like COPD. This blurs the line even more.
What You Can Do
If you’re struggling to breathe:
- Track your symptoms. When do they happen? At night? After exercise? All the time?
- Know your history. Did you have asthma as a child? Have you smoked for years?
- Get tested. Spirometry, FeNO, and blood eosinophil counts can clarify what’s going on.
- Quit smoking-even if you’re not sure it’s COPD. It’s the single best thing you can do for your lungs.
Don’t assume your symptoms are "just asthma" if you’re over 40 and smoke. And don’t dismiss breathing trouble as "just aging" if you’ve never smoked. The right diagnosis changes everything.
Can asthma turn into COPD?
Asthma doesn’t directly turn into COPD. But long-term, poorly controlled asthma-especially in smokers-can lead to permanent lung changes that look like COPD. About 15-20% of people with asthma for over 20 years develop fixed airflow obstruction. This is why quitting smoking and managing asthma early is so important.
Is COPD curable?
No, COPD is not curable. The lung damage it causes is permanent. But it can be managed. Quitting smoking, using bronchodilators, doing pulmonary rehab, and avoiding triggers can slow progression, reduce flare-ups, and help you stay active longer. Early diagnosis and consistent treatment make a big difference in quality of life.
Can you have asthma and COPD at the same time?
Yes. This is called Asthma-COPD Overlap Syndrome (ACOS). It affects 15-25% of people with obstructive lung disease. These patients have features of both conditions-like reversible airflow obstruction and persistent airway damage. Diagnosis requires careful testing, including spirometry, FeNO, and blood eosinophil counts. Treatment often combines asthma and COPD medications.
Why do some asthma patients need steroids daily?
Asthma is driven by chronic airway inflammation, often from allergies or immune overreactions. Inhaled corticosteroids reduce that inflammation at the source. If you’re having symptoms more than twice a week, or waking up at night because of breathing issues, daily steroids help prevent attacks. They’re not addictive-they’re maintenance medicine, like blood pressure pills.
How do I know if my inhaler is working?
If you’re using a rescue inhaler (like albuterol) more than twice a week for symptoms, it’s not working well enough. That’s a sign your asthma or COPD isn’t controlled. You may need a daily controller medication. Also, if you’re still coughing, wheezing, or getting winded doing normal activities, talk to your doctor. The goal isn’t just to survive-it’s to live without limits.

10 Comments
February 12, 2026 Gloria Ricky
I had no idea asthma could be so reversible. My mom’s been on inhalers for 20 years and I always thought it was just "bad lungs." But reading this makes me realize she might’ve been under-treated. I’m gonna ask her doctor about FeNO testing. This info is gold.
February 13, 2026 Neha Motiwala
I’ve been told I have asthma since I was 8 but I’ve never had a single spirometry test. The doctor just looked at me and said "you’re wheezing so it’s asthma." Now I wonder if I actually have ACOS and they just gave me the easy label. I’ve been smoking since 19 and I’m 32. Maybe I’m one of those 15-20% who turned asthma into COPD without knowing it. Scary.
February 14, 2026 Jack Havard
The data here is solid but I’ve seen too many patients get misdiagnosed because doctors skip the basics. I’m not saying this is wrong, but I’ve seen spirometry done wrong, FeNO machines miscalibrated, and eosinophil counts ignored because it’s "easier" to prescribe an ICS and call it asthma. The system’s broken.
February 15, 2026 Annie Joyce
COPD patients aren’t just smokers who got lazy-they’re people who started with a job in a factory, or a kitchen, or a dusty warehouse, and no one ever told them the air they breathed was slowly killing them. This isn’t just about lungs. It’s about who gets warned, and who gets left behind.
February 16, 2026 Alyssa Williams
If you're using your rescue inhaler more than twice a week you're not managing it you're surviving it
February 17, 2026 Stacie Willhite
I’ve been in the ER three times for "asthma attacks" and they all turned out to be anxiety. But reading this made me realize maybe it wasn’t anxiety-maybe it was early COPD. I never smoked but my dad did. I grew up in the smoke. I’m getting tested next week.
February 18, 2026 Rob Turner
I’ve worked in UK public health for 18 years. The real tragedy isn’t misdiagnosis-it’s that COPD screening isn’t routine for anyone over 40 with a smoking history. We screen for colon cancer at 50. Why not lungs? We’re letting people die slowly because we don’t want to face the cost.
February 19, 2026 christian jon
This whole article is a Big Pharma playbook. Inhaled steroids? Biologics? Triple therapy? You’re being sold a $10,000/year treatment plan for a problem that could be solved with clean air, diet, and breathing exercises. The lung damage? It’s not irreversible-you’re just being told it is because they can’t sell you a cure. Wake up.
February 20, 2026 Jason Pascoe
I’ve got ACOS. I’m 47, smoked for 15 years, had asthma as a kid. Triple therapy helps-but pulmonary rehab changed my life. I can now carry groceries without stopping. It’s not glamorous. But it’s real. If you’re reading this and you’re wheezing-find a rehab program. It’s free in most places.
February 21, 2026 athmaja biju
In India we have no access to FeNO or spirometry in 80% of villages. People die with a cough and a belief that it’s "just a cold." This article is useful for clinics in New York-but for the millions in rural India? It’s a luxury. We need low-cost, portable diagnostics-not fancy tests.
Write a comment