What Happens When Your Heart Skips a Beat?
Your heart isn’t supposed to race, flutter, or pause randomly. When it does, that’s an arrhythmia - and it’s more common than you think. About 1 in 4 adults will develop atrial fibrillation (AF) by age 80. For many, medications help. But for others, drugs just don’t cut it. That’s where catheter ablation and device therapy come in. These aren’t last-resort options anymore. They’re now frontline treatments for people who are tired of feeling like their heart is out of control.
Let’s cut through the noise. This isn’t about theory. It’s about what actually works, what the data says, and what real patients experience after the procedure.
Catheter Ablation: How It Fixes a Faulty Wiring System
Think of your heart like a house with faulty electrical wiring. Sometimes, extra signals start firing in the wrong places - usually near the pulmonary veins in the left atrium. These rogue signals trigger AF, causing that chaotic fluttering feeling. Catheter ablation doesn’t fix the whole system. It targets the exact spots causing the problem.
The procedure starts with a tiny incision in the groin. A thin, flexible tube - a catheter - is threaded up into your heart. Using real-time 3D mapping, the doctor finds the problem zones. Then, energy is delivered to scar those areas just enough to block the abnormal signals. No open surgery. No big scars. Most people go home the same day or the next.
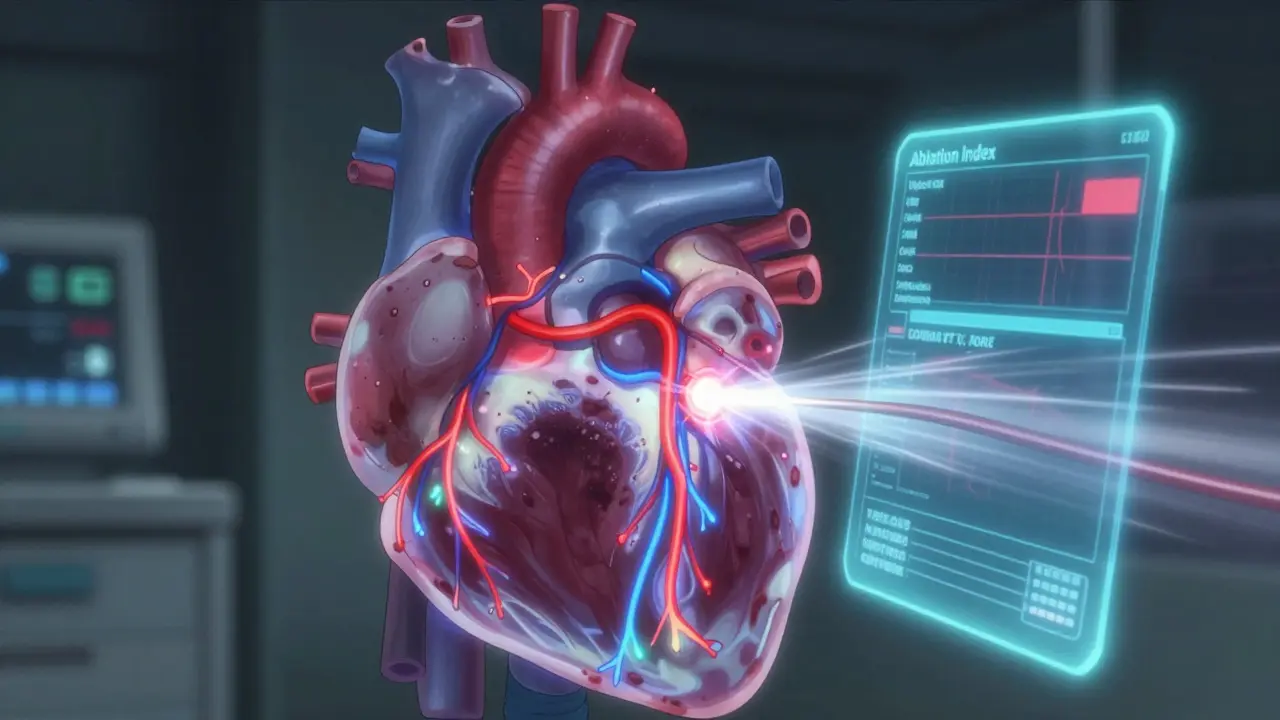
There are two main types of energy used today: radiofrequency (heat) and cryoablation (freezing). Radiofrequency uses controlled heat to burn the tissue. Cryoablation uses a balloon filled with freezing gas to freeze the tissue around the pulmonary veins. Both are effective, but they work differently.
Radiofrequency ablation takes longer - about 2.5 to 3 hours - but gives the doctor more control. Cryoablation is faster, around 90 to 120 minutes, and simpler to perform. That’s why many centers now use cryoablation as the go-to for paroxysmal AF. For persistent AF, radiofrequency is still the standard because it allows more precise lesion placement.
The big breakthrough? Contact force sensing. Older catheters couldn’t tell if they were pressing hard enough against the heart wall. Too light? The lesion doesn’t form. Too hard? You risk tearing tissue. New catheters like the THERMOCOOL SMARTTOUCH measure pressure in real time. They even calculate an Ablation Index - a score that combines pressure, time, and power to predict how deep and lasting the scar will be. Studies show this cuts recurrence rates by 12-15% compared to older tools.
Device Therapy: When the Heart Needs a Pacemaker or ICD
Ablation fixes the signal. But sometimes, the heart’s natural pacemaker is broken. That’s where device therapy comes in.
For slow heart rhythms (bradycardia), a pacemaker is implanted under the skin in the chest. It sends tiny electrical pulses to keep the heart beating regularly. Modern pacemakers are tiny - about the size of a stopwatch - and last 7 to 10 years. Many can now monitor your heart rhythm remotely, sending alerts to your doctor if something’s off.
For fast, dangerous rhythms like ventricular tachycardia or fibrillation, an implantable cardioverter-defibrillator (ICD) is used. It doesn’t just pace - it can deliver a life-saving shock if your heart goes into cardiac arrest. These devices are more complex and are recommended for people with heart failure, especially those with reduced ejection fraction (HFrEF).
Here’s the kicker: for patients with both AF and HFrEF, catheter ablation doesn’t just improve rhythm - it improves survival. A 2019 meta-analysis in Circulation: Arrhythmia and Electrophysiology found a 48% drop in death risk after ablation compared to meds alone. That’s not a small number. That’s life-changing.
ICDs and pacemakers aren’t perfect. They can cause infections. They can deliver shocks when they shouldn’t. But for high-risk patients, the benefit outweighs the risk. In fact, the latest guidelines say ICDs should be offered to anyone with HFrEF and AF who’s at risk of sudden cardiac arrest.

Ablation vs. Medication: The Numbers Don’t Lie
For years, doctors told people with AF to just take pills. Antiarrhythmic drugs like amiodarone or flecainide. But those drugs have side effects - thyroid problems, lung damage, liver issues. And they often stop working over time.
A 2020 review of 1,797 patients showed ablation reduced AF recurrence by 58% compared to drugs. That’s more than half. It also cut hospital visits for heart problems by 44%. For someone who’s had multiple ER trips because their heart went haywire, that’s huge.
And it’s not just about rhythm. People who get ablation feel better. A 2023 JAMA study found those who had ablation had significantly lower levels of anxiety and depression. Why? Because they weren’t constantly wondering if the next flutter was going to be the one that sent them to the hospital.
One patient, John M., 58, from Bristol, had AF for 8 years. He was on three drugs. Still felt tired. Couldn’t cycle like he used to. After cryoablation in March 2022? No AF. No meds. Back on his bike in three months. He told his doctor, “I didn’t realize how much I’d been holding my breath.”
What About the Risks?
No procedure is risk-free. About 8% of people have a major complication from ablation. The most serious? Cardiac tamponade - bleeding around the heart. It happens in about 1.2% of cases. It’s rare, but it needs immediate treatment.
Cryoablation carries a small risk of injuring the phrenic nerve - the nerve that controls the diaphragm. That can cause shortness of breath. But doctors now use pacing during the procedure to test the nerve in real time. If it starts to weaken, they stop before damage is done.
Another issue? Incomplete lesions. If the catheter doesn’t touch the tissue properly, the scar doesn’t form. That’s why contact force catheters are now standard. They reduce this risk by 35%.
Recovery takes time. Most people take it easy for a week. Some feel chest discomfort or irregular beats for a few weeks - that’s normal. But if you have fever, swelling, or sudden shortness of breath, call your doctor. Don’t wait.
Who Gets Ablation? And Who Doesn’t?
The guidelines are clear. If you have paroxysmal AF (episodes that come and go) and one antiarrhythmic drug didn’t work, ablation is now a first-line option. Not second. First.
For persistent AF (AF that lasts more than a week), ablation is still recommended - but the success rate is lower. Around 60-70% after one procedure. Many need a second one. That’s why doctors now talk about “ablation as a process,” not a one-time fix.
But not everyone qualifies. If you have a very enlarged heart, severe valve disease, or have been in AF for over 10 years, ablation is less likely to help. The longer the heart has been in AF, the more it changes structurally. That’s why early intervention matters.
Device therapy is for different people. If you have a slow heart rate or are at risk of sudden death, a pacemaker or ICD might be your best bet - even if you still have AF.
The Future: Pulsed Field Ablation and AI
The next big thing? Pulsed field ablation (PFA). Instead of heat or cold, it uses short bursts of electric pulses to kill heart cells - but only heart cells. It doesn’t damage nearby nerves or the esophagus. That’s huge. The Farapulse system got FDA approval in September 2023. In trials, it had 86% success at 12 months and took just 76 minutes - half the time of traditional ablation.
And it’s getting smarter. Medtronic is rolling out AI software in 2025 that analyzes the heart’s electrical patterns in real time and suggests where to ablate. It’s like having a co-pilot in the lab.
By 2030, the Heart Rhythm Society predicts ablation will be the first choice for nearly all symptomatic AF patients. Not because it’s trendy. Because the data proves it saves lives.
Cost, Access, and Real-World Barriers
Let’s be honest. Ablation isn’t cheap. In the U.S., it costs between $16,000 and $21,000. In the UK, it’s covered by the NHS, but wait times can be long. In rural areas, access is still limited. About 60% fewer hospitals in small towns have the equipment or trained staff.
But here’s the twist: over time, ablation saves money. After 3 to 8 years, the cost of repeated hospital visits, ER trips, and meds adds up to more than the procedure. One study found ablation paid for itself in under five years.
And adoption is growing fast. In 2015, only 35% of European centers offered ablation as a first-line option. By 2023, that jumped to 78%.
What Should You Do Next?
If you’re on meds and still feel your heart racing, fluttering, or skipping - talk to your cardiologist. Ask if you’re a candidate for ablation. Bring your symptom diary. How often do you have episodes? How long do they last? Do they interfere with sleep, work, or exercise?
If you have heart failure and AF, don’t wait. The survival benefit is real. The sooner you get evaluated, the better your outcome.
Ablation isn’t magic. It’s medicine - precise, evidence-based, and life-changing for the right person.
Is catheter ablation painful?
Most people feel little to no pain during the procedure because they’re sedated. You might feel pressure when the catheters are moved, but not sharp pain. Afterward, there’s mild soreness in the groin where the catheter was inserted, and some people report chest discomfort for a few days. That’s normal. Severe pain is rare and should be reported immediately.
How long does it take to recover from ablation?
Most people return to light activities within 3-5 days. Avoid heavy lifting or strenuous exercise for 1-2 weeks. It can take up to 3 months for the heart to fully heal and for the ablation scars to stabilize. During this time, you might still feel occasional palpitations - that doesn’t mean the procedure failed. It’s part of the healing process.
Will I still need medication after ablation?
Some people can stop all antiarrhythmic drugs after a successful ablation. Others still need blood thinners like warfarin or apixaban to prevent stroke, especially if they have other risk factors like high blood pressure or diabetes. Your doctor will monitor your rhythm and adjust meds based on your results.
Can ablation cure atrial fibrillation?
It’s not a guaranteed cure, but it’s the most effective treatment for symptom control. For paroxysmal AF, about 70-80% of patients are free from AF after one procedure. For persistent AF, it’s around 60%. Many need a second ablation for better results. Even if AF returns, the episodes are usually less frequent and less severe.
What’s the difference between a pacemaker and an ICD?
A pacemaker treats slow heart rates by sending small electrical pulses to keep your heart beating regularly. An ICD does that too, but it can also deliver a strong shock if your heart goes into a life-threatening fast rhythm like ventricular fibrillation. ICDs are for people at risk of sudden cardiac arrest; pacemakers are for those with slow rhythms or conduction problems.
Are there alternatives to ablation and devices?
Medications are the main alternative, but they often don’t work well long-term and come with side effects. Surgical maze procedures exist but are much more invasive - only used in rare cases, usually during open-heart surgery for other reasons. For most people, ablation or device therapy is the best next step after drugs fail.

10 Comments
January 22, 2026 Darren Links
So let me get this straight - we’re now treating heart rhythm issues like we’re fixing a Wi-Fi router? Just zap the bad spots and boom, instant connection? Meanwhile, my cousin got a pacemaker and now his heart beats like a metronome set to ‘boring.’ This whole ablation thing feels like tech bro medicine - all flash, no substance.
January 22, 2026 Jamie Hooper
mate i had the cryo thing last year and honestly? best decision ever. no more panic attacks every time i climb stairs. felt like my heart was gonna explode outta my chest. now i can drink beer on the sofa without checking my pulse. 10/10 would do again. they stuck a catheter up my leg and i napped through it. magic.
January 23, 2026 Elizabeth Cannon
For anyone reading this and scared - you’re not alone. I was terrified of ablation too. But after 5 years of AF and 3 meds that made me feel like a zombie, I did it. Recovery was rough for a week, but now I sleep through the night. My kid says I’m ‘less grumpy.’ That’s worth it. Talk to your doc. Don’t wait till you’re in the ER again.
January 24, 2026 Marlon Mentolaroc
Let’s crunch some real numbers. Ablation costs $18k. ER visits for AF episodes? $1.2k each. Avg patient has 3.7 per year. That’s $4,440/year. Break-even at 4 years. Add in lost productivity, missed work, anxiety meds - you’re saving $12k+ over 5 years. This isn’t hype. It’s actuarial science. Stop being emotional about your heart. Do the math.
January 24, 2026 Shelby Marcel
Wait so if pulsed field ablation only kills heart cells and not nerves... does that mean it doesn’t hurt the esophagus? Because I heard someone got a hole in their esophagus after ablation and it was wild. Like, they had to have surgery to fix it. Is PFA really safer? Or is that just the marketing?
January 25, 2026 blackbelt security
I’m a paramedic. Saw a guy come in with a defib shock mark on his chest. Asked him why. He said, ‘I ignored the fluttering for 2 years.’ Dude, your heart doesn’t need to be a superhero. It just needs to work. If you feel off - get checked. Don’t be the guy who waits until the machine saves you.
January 25, 2026 Patrick Gornik
The entire paradigm of cardiac intervention is a neoliberal fantasy of technological redemption. We’ve outsourced bodily sovereignty to the cath lab, commodifying rhythm as a variable to be optimized. Pulsed field ablation? Merely the latest epistemic rupture in the medical-industrial complex’s endless quest for algorithmic control over the animate. The heart isn’t a circuit - it’s a metaphysical signature. And yet, we reduce it to ablation indices and contact force metrics. We are not healing. We are engineering surrender.
January 27, 2026 asa MNG
Uhhh… did you know the FDA approved ablation devices after like 2 guys in a lab said ‘it looks good’? And now everyone’s getting zapped? I heard the catheters are made in China and sometimes the wire snaps inside you. Like, literally. And they just leave it there. 🤯 My neighbor’s aunt had a piece of catheter stuck in her heart for 3 years. No one told her. 😳
January 28, 2026 Chloe Hadland
I’m just glad this info is out there. I’ve been feeling off for months but didn’t know if it was stress or my heart. Reading this made me finally call my doctor. No panic, no drama - just ‘hey, can we talk about this?’ And guess what? He didn’t laugh. He said ‘let’s check.’ That’s all I needed. 💙
January 30, 2026 Dolores Rider
I think they’re hiding something. Why is this only available in big cities? Why do rural hospitals say ‘we don’t have the equipment’? Coincidence? Or is Big Pharma pushing meds because they make more money? And why does every ad for ablation show happy white people on bikes? Who’s paying for this narrative? 🤔
Write a comment