What is hypoparathyroidism?
Hypoparathyroidism is a rare endocrine disorder where the parathyroid glands don’t make enough parathyroid hormone (PTH). Without enough PTH, your body can’t regulate calcium and phosphate properly. Blood calcium drops too low (hypocalcemia), and phosphate builds up (hyperphosphatemia). This isn’t just a lab abnormality-it causes real symptoms like tingling in the fingers, muscle cramps, fatigue, and even seizures if left untreated.
Most cases happen after thyroid or neck surgery, where the parathyroid glands get accidentally damaged or removed. About 75-90% of cases are surgical. Other causes include autoimmune diseases, genetic conditions like DiGeorge syndrome, or radiation treatment. No matter the cause, the result is the same: your body loses its natural way to keep calcium balanced.
Why calcium and vitamin D matter so much
PTH normally tells your bones to release calcium, your kidneys to hold onto calcium, and your gut to absorb more from food. Without it, calcium leaks out in urine, bones don’t give up their stores, and your intestines can’t absorb what you eat. That’s why treatment focuses on replacing what PTH can’t do: calcium and active vitamin D.
Here’s the catch: regular vitamin D (cholecalciferol) won’t cut it. Your kidneys need PTH to convert it into the active form. So doctors prescribe calcitriol or alfacalcidol-active vitamin D analogues that bypass this step. These work faster and more reliably than plain vitamin D. In fact, studies show calcitriol raises calcium levels 2.3 times quicker than cholecalciferol.
You’ll also need calcium supplements. Most doctors start with calcium carbonate because it’s cheap and contains 40% elemental calcium. That means you need less of it to get the same effect. For example, 1,250 mg of calcium carbonate gives you 500 mg of actual calcium. Some people take calcium citrate instead, especially if they have low stomach acid, but you’d need nearly twice as much to get the same dose.
Typical treatment plan: Dosing and timing
There’s no one-size-fits-all dose, but most people start with:
- Calcium: 1,000-2,000 mg daily, split into 2-4 doses
- Active vitamin D: 0.25-0.5 mcg of calcitriol or alfacalcidol daily
- Regular vitamin D3: 400-800 IU daily to keep 25-hydroxyvitamin D between 20-30 ng/mL
Timing matters. Take calcium supplements with meals-it helps absorption and acts as a phosphate binder, reducing how much phosphorus your body absorbs. Vitamin D is often taken at bedtime because it’s fat-soluble and absorbs better with overnight digestion.
Don’t take calcium and vitamin D at the same time as iron or thyroid meds-they interfere. Space them out by at least 4 hours.
What to aim for: Blood and urine targets
The goal isn’t to push calcium into the normal range-it’s to keep it in the lower half to protect your kidneys. Experts recommend:
- Serum calcium: 2.00-2.25 mmol/L (8.0-8.5 mg/dL)
- 24-hour urinary calcium: Less than 250 mg (6.25 mmol)
- Serum phosphate: 2.5-4.5 mg/dL
- Magnesium: Above 1.7 mg/dL
Why focus on urine calcium? Too much calcium in your urine leads to kidney stones and long-term kidney damage. About 35-40% of patients develop this problem even on standard doses. That’s why doctors check your 24-hour urine before increasing any meds.
Magnesium is often overlooked. If your magnesium is low, your body can’t respond to PTH-even if you’re taking supplements. If magnesium falls below 1.7 mg/dL, start 400-800 mg of magnesium oxide or citrate daily. Many patients feel better once this is fixed.

When standard treatment fails
Most people (60-70%) do fine with calcium and vitamin D. But about 25-30% struggle. You might be in this group if:
- You need more than 2,000 mg of calcium daily
- You need more than 2 mcg of active vitamin D daily
- You still have high urine calcium despite max doses
- You’re constantly tired, tingling, or cramping
For these patients, doctors may consider recombinant human PTH(1-84) (Natpara) or teriparatide (Forteo). These are daily injections that mimic natural PTH. They can cut calcium and vitamin D needs by 30-40%. But they’re expensive-Natpara costs about $15,000 a month-and require special handling through a REMS program. Insurance approval can take 30-45 days.
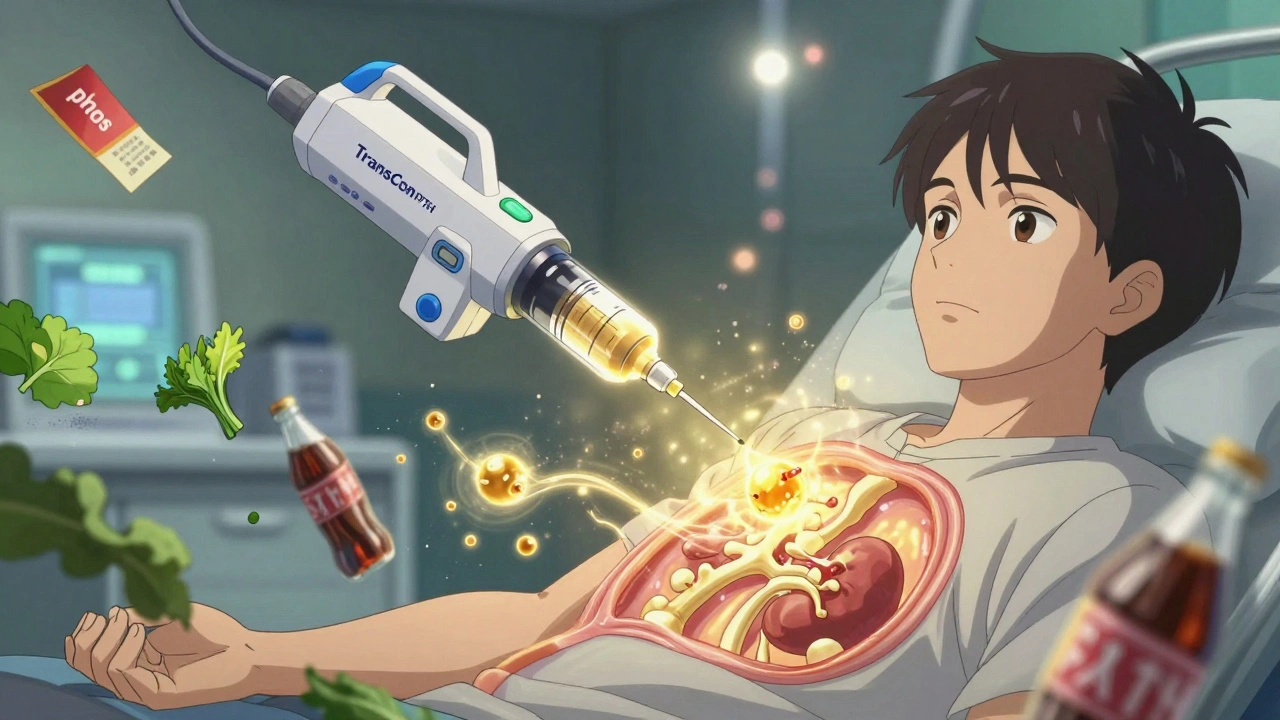
There’s also a new drug in the pipeline: TransCon PTH. In a 2022 trial, it normalized calcium in 89% of patients with just one injection a day. It’s not approved yet, but it could be a game-changer for people tired of taking 6-10 pills a day.
Dietary tips: What to eat and avoid
Diet plays a big role. You need calcium-rich foods, but you also have to limit phosphorus.
Good sources of calcium:
- Dairy: Milk, yogurt, cheese (300 mg per serving)
- Leafy greens: Kale (100 mg per cup), broccoli (43 mg per cup)
- Fortified foods: Plant milks, tofu, orange juice
Phosphorus to avoid:
- Cola drinks: 500 mg per liter
- Processed meats: 150-300 mg per serving
- Hard cheeses: 500 mg per ounce
- Fast food and packaged snacks: Often loaded with phosphate additives
Stick to whole, unprocessed foods. Read labels for “phos” or “phosphate” in ingredients. Even if a food looks healthy, it might be loaded with hidden phosphorus.
Also, limit sodium to under 2,000 mg a day. High salt makes your kidneys dump more calcium into urine. A low-sodium diet can help reduce urinary calcium without cutting calcium intake.
Common problems and how to fix them
Many patients report a “calcium rollercoaster”-feeling fine one day, then tingling and shaky the next. This often happens because doses aren’t spread out enough. Try splitting calcium into 4-5 smaller doses instead of 2-3 big ones. Many patients say this smooths out their symptoms.
Constipation is another big issue. High-dose calcium slows digestion. Increase water, fiber, and movement. If that doesn’t help, talk to your doctor about switching to calcium citrate-it’s gentler on the gut.
Some people develop kidney stones. If that happens, your doctor might add a thiazide diuretic like hydrochlorothiazide (12.5-25 mg daily). It helps your kidneys reabsorb calcium instead of losing it.
And don’t ignore magnesium. Low magnesium is a silent culprit behind stubborn low calcium. Get it checked every 3-6 months.
Long-term risks and monitoring
Hypoparathyroidism isn’t just about feeling better today-it’s about protecting your body for decades. Studies show that 15-20% of patients develop chronic kidney disease after 10 years on conventional therapy. And if your calcium stays above 2.35 mmol/L for years, you’re 2.8 times more likely to get calcium deposits in your brain (basal ganglia calcification), which can cause movement problems or seizures.
That’s why regular blood and urine tests are non-negotiable. In the first 3 months, you’ll need visits every 2-4 weeks. Once stable, 3-4 visits a year are enough. But if you’re on PTH replacement or have kidney issues, you’ll need more frequent checks.
Always carry emergency calcium. If you feel sudden numbness, muscle spasms, or chest tightness, chew 2-3 calcium tablets right away. Don’t wait. Call your doctor after.
Who manages your care?
Most patients start with an endocrinologist. But once stable, your primary care doctor can handle routine checks-with endocrinology backup for complications. The problem? A 2021 survey found 78% of family doctors feel undertrained in hypoparathyroidism. That’s why patient advocacy groups like Parathyroid UK and the Hypopara Alliance offer resources and support.
Join a patient community. Reddit’s r/Hypoparathyroidism has over 1,200 members sharing tips on dosing, insurance battles, and symptom tracking. You’re not alone. And you don’t have to figure this out by yourself.
What’s next for treatment?
The future is moving beyond pills. TransCon PTH could mean one injection a week instead of daily pills. Gene therapies targeting the calcium-sensing receptor are in early animal trials. Human trials won’t start before 2026, but they offer hope for a cure, not just management.
For now, the best thing you can do is stick to your plan, track your symptoms, and speak up if something feels off. Your body’s calcium balance is delicate-but with the right approach, you can live well, even with hypoparathyroidism.
Can I take regular vitamin D instead of calcitriol for hypoparathyroidism?
No. Regular vitamin D (cholecalciferol) needs PTH to be activated in the kidneys. In hypoparathyroidism, that step doesn’t work. You must take active forms like calcitriol or alfacalcidol. These bypass the blocked step and directly raise calcium levels. Using regular vitamin D won’t help and may delay proper treatment.
Why is my calcium level still low even though I’m taking supplements?
Low magnesium is a common reason. Magnesium helps your body respond to PTH and absorb calcium. If your magnesium is below 1.7 mg/dL, supplements won’t work well. Get your levels checked. Also, check if you’re taking calcium with meals-without food, absorption drops sharply. And make sure you’re not taking calcium with iron, thyroid meds, or antacids-they interfere.
Can hypoparathyroidism be cured?
Not yet. Most cases are permanent, especially after surgery. But new treatments like TransCon PTH are showing promise in clinical trials. These aim to replace PTH naturally, not just manage symptoms. While a true cure isn’t available today, the goal is to reduce pill burden and prevent long-term damage. Research is advancing quickly.
Is it safe to take high doses of calcium long-term?
It’s safe if your urine calcium is monitored. High calcium intake increases kidney stone and heart disease risk-but only if you’re also excreting too much calcium in urine. That’s why doctors test 24-hour urine before increasing doses. If your urine calcium is under 250 mg/day, you’re likely safe. If it’s higher, your doctor may lower your calcium dose, add a thiazide diuretic, or switch to PTH therapy.
What should I do if I miss a dose of calcium or vitamin D?
If you miss a calcium dose, take it as soon as you remember-but not right before bed. If it’s close to your next dose, skip it. Don’t double up. For vitamin D, missing one dose isn’t critical since it builds up over time. But calcium needs to be taken consistently with meals. If you’re feeling tingling or cramping after missing doses, chew 500-1,000 mg of calcium immediately and contact your doctor.
Can I stop taking supplements if I feel fine?
Absolutely not. Hypoparathyroidism is a lifelong condition. Even if you feel fine, your body still lacks PTH. Stopping supplements will cause calcium to drop, and symptoms can return quickly-even dangerously. Many patients feel fine for months, then suddenly have a seizure because they skipped doses. Never stop without your doctor’s guidance.
Next steps: What to do now
If you’ve just been diagnosed:
- Get a 24-hour urine calcium test before starting treatment.
- Ask for serum magnesium and phosphate levels.
- Start calcium carbonate with meals and calcitriol at bedtime.
- Join a patient group like Parathyroid UK or Hypopara Alliance.
- Keep a symptom and dose log-this helps your doctor adjust faster.
If you’ve been on treatment for years and still feel off:
- Check your magnesium and urine calcium-most doctors don’t test these often enough.
- Ask if splitting calcium into 4-5 doses might help.
- Discuss PTH replacement if you’re on high doses.
- Review your diet for hidden phosphorus.
Hypoparathyroidism is manageable. It’s not easy-but with the right plan, you can live without constant symptoms and protect your long-term health.


12 Comments
December 9, 2025 Elliot Barrett
This is the most useless wall of text I've read all week. I skipped half of it. Just tell me what to take and when.
December 9, 2025 Tejas Bubane
The fact that you're recommending calcium carbonate over citrate without addressing gastric acid sufficiency is amateur hour. Most hypoparathyroid patients have atrophic gastritis post-thyroidectomy. You're setting people up for malabsorption and failed therapy. Basic physiology.
December 10, 2025 Ajit Kumar Singh
Listen here i been living with this for 15 years and let me tell you something nobody talks about the magnesium thing is real i was in the ER three times with cramps and turns out my mg was 1.4 they never checked it until i screamed at my doc and now im on 800mg a day and i feel like a new person stop ignoring magnesium its not optional its survival
December 11, 2025 Maria Elisha
I just started this and honestly I’m already overwhelmed. Like, 10 pills a day? And I have to time them with meals? And avoid phosphorus? I didn’t even know soda had phosphate in it. This is exhausting.
December 13, 2025 Angela R. Cartes
I appreciate the effort, but the fact that you mention Natpara at $15k/month without acknowledging insurance gatekeeping is tone-deaf. Most of us are stuck on the pill treadmill because we can’t even get the paperwork approved. This reads like a textbook written by someone who’s never had to fight a prior authorization.
December 13, 2025 Andrea Beilstein
It's interesting how we treat this as a biochemical problem when it's really a metaphysical one. The parathyroid isn't just a gland-it's the body's silent architect of balance. We're not just replacing calcium, we're trying to reconstruct a lost harmony. The pills are just symbols of a deeper rupture. And yet... we persist. There's poetry in that.
December 15, 2025 Lisa Whitesel
People who don't take their meds consistently deserve every seizure they get. This isn't a suggestion, it's a biological contract. Miss a dose? You're gambling with your brain. Stop acting like this is optional.
December 15, 2025 Larry Lieberman
Just read the TransCon PTH trial results 😍 One shot a day and 89% normocalcemia? That’s like a sci-fi movie becoming real. When’s it coming to my pharmacy?? 🤯
December 16, 2025 Sabrina Thurn
The 24-hour urinary calcium metric is non-negotiable. Without it, you're managing symptoms, not pathology. I've seen too many patients develop nephrocalcinosis because their clinicians prioritized serum calcium over renal excretion. Always order the 24-hour urine before escalating therapy. It's the only way to avoid iatrogenic kidney injury.
December 16, 2025 Courtney Black
I used to think hypoparathyroidism was just about calcium. Then I realized it’s about control. Control over your body, over your time, over your food, over your sleep, over your emotions. You’re not just managing a hormone-you’re managing a life that’s been hijacked by a system that doesn’t care if you’re tired. And yet, you keep taking the pills. That’s not compliance. That’s heroism.
December 17, 2025 iswarya bala
omg i just found this post and i was crying because i thought i was the only one who gets cramps at 3am and no one believes me lol thanks for the magnesium tip i just got my test done and its low as hecklll i’ll start taking it tomorrow
December 17, 2025 Elliot Barrett
I’m the OP. Thanks for the feedback. I’ll add a note about magnesium testing being mandatory before any dose adjustments. Also, for those asking about insurance: I’ve been through the Natpara nightmare too. The key is having your endo write a detailed letter using the phrase 'failure of conventional therapy'-that’s what triggers the appeal.
Write a comment