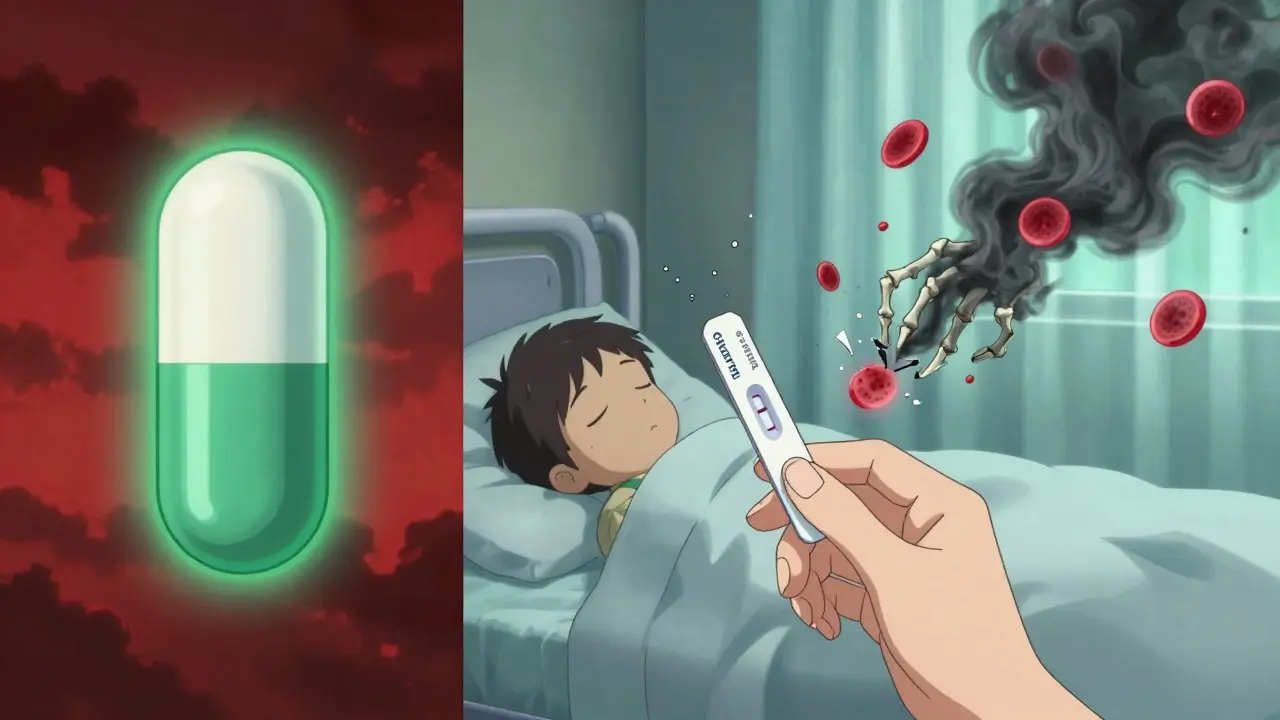
Every year, millions of people take nitrofurantoin to treat a simple urinary tract infection (UTI). It works fast, it’s cheap, and for most people, it’s safe. But for a surprising number of others, this common antibiotic can trigger a life-threatening reaction they never saw coming: hemolytic anemia.
What Happens When Nitrofurantoin Meets G6PD Deficiency?
Nitrofurantoin doesn’t just kill bacteria-it creates oxidative stress. In healthy people, red blood cells handle this just fine. They have a built-in defense system powered by an enzyme called glucose-6-phosphate dehydrogenase (G6PD). This enzyme keeps glutathione levels up, which protects hemoglobin from damage. But if you have G6PD deficiency, that defense is broken. You don’t make enough of the enzyme. When nitrofurantoin enters your system, it overwhelms your red blood cells. Hemoglobin starts to clump, cells burst, and your body can’t replace them fast enough. That’s hemolytic anemia. Symptoms show up fast-usually within 24 to 72 hours of taking the first pill. You might feel feverish, dizzy, or short of breath. Your urine turns dark, your skin yellows, and your heart races. In severe cases, you’ll need hospital care. Some patients have died from it.Who’s at Risk?
G6PD deficiency isn’t rare. It affects around 400 million people worldwide. And it’s not random. It’s tied to ancestry. - People of African descent: 10-14% carry the gene - People from the Mediterranean or Middle East: 4-7% - People from Southeast Asia: 2-5% In the U.S., Black and African American patients are most likely to be undiagnosed carriers. Many don’t know they have it until they take nitrofurantoin-or another oxidant drug like sulfamethoxazole or primaquine-and their body reacts. Pregnant women and newborns are especially vulnerable. There are documented cases where mothers taking nitrofurantoin passed the reaction to their babies. Infants exposed in utero or through breast milk have developed severe hemolysis. The American Society of Hematology says this is a hard no for G6PD-deficient pregnant women.Why Do Doctors Still Prescribe It?
It’s not that doctors are ignoring the risk. They’re balancing trade-offs. Nitrofurantoin works well against E. coli, the most common cause of UTIs. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), another first-line option, is climbing-up to 25% in some areas. Nitrofurantoin resistance? Still under 15%. It’s also cheaper than newer antibiotics like fosfomycin or cefdinir. But here’s the problem: most doctors don’t screen for G6PD deficiency before prescribing. A 2022 survey of 350 primary care providers found only 32% routinely test for it. Even though the CPIC (Clinical Pharmacogenetics Implementation Consortium) and the FDA both warn about the risk, there’s no legal requirement to test. The FDA label says: “Hemolytic anemia has been reported in G6PD-deficient individuals.” That’s it. No mandate. No checklist. No alert built into most electronic health records.
The Cost of Skipping the Test
G6PD testing costs between $35 and $50. A simple finger-prick blood test. Results in under an hour with newer point-of-care devices. Now compare that to the cost of a hospital admission for drug-induced hemolytic anemia: $8,500 to $12,000. That’s not even counting lost wages, time off work, or the emotional toll. One 2023 case study in the NCBI describes a patient who took nitrofurantoin for a UTI. Within two days, his hemoglobin dropped from 14 g/dL to 7.2 g/dL. His bilirubin soared. His LDH was through the roof. He was hospitalized, given IV fluids, and recovered fully in 48 hours after stopping the drug. No transfusion needed. But he was lucky. Ten deaths from nitrofurantoin-induced hemolysis have been recorded in pharmacovigilance databases. All were preventable.What Should You Do?
If you’re being prescribed nitrofurantoin, ask these questions:- Do I have G6PD deficiency?
- Have I been tested before?
- What’s my ancestry? Am I from Africa, the Mediterranean, or Southeast Asia?
- Are there safer alternatives?
Alternatives to Nitrofurantoin
If you have G6PD deficiency-or if your doctor isn’t sure-there are other options:- Fosfomycin: Single-dose oral antibiotic. Safe for G6PD-deficient patients. First-line in Europe for uncomplicated UTIs.
- Cephalexin: A cephalosporin. Low risk of hemolysis. Good for patients with normal kidney function.
- Pivmecillinam: Used widely in Europe. Not available in the U.S. yet, but under review.
- Trimethoprim-sulfamethoxazole: Avoid if you have G6PD deficiency. Sulfonamides are also oxidants.
Why Isn’t This Standard Practice?
The biggest barrier? Lack of awareness-and inertia. Many doctors assume G6PD deficiency is rare. It’s not. In urban clinics with high African or Middle Eastern patient populations, up to 1 in 10 people may be carriers. Testing isn’t always covered by insurance. Some labs require pre-authorization. Point-of-care devices aren’t common in primary care offices. And here’s the cruel irony: if you’re a woman with a UTI, your doctor might prescribe nitrofurantoin without even asking your name. It’s automatic. But if you’re a Black man with the same infection, you’re more likely to be tested for diabetes or kidney disease than for G6PD deficiency.What’s Changing?
Change is coming-but slowly. The CPIC updated its guidelines in 2023 to clearly say: avoid nitrofurantoin in G6PD-deficient patients with chronic hemolytic anemia. For others, use with caution. That’s a step forward. The NIH is running a trial (NCT04567891) to see if routine G6PD testing before nitrofurantoin use saves money and lives. Results are due in mid-2024. Point-of-care tests are getting cheaper and faster. Some clinics in the UK and Australia are already using them in urgent care settings. And the market is responding. The global G6PD testing market is projected to grow from $185 million in 2022 to over $310 million by 2027. That’s not because people are suddenly more health-conscious. It’s because more people are dying from preventable drug reactions.The Bottom Line
Nitrofurantoin isn’t evil. It’s a useful tool. But like any tool, it can hurt you if you don’t know how to use it safely. If you’re prescribed nitrofurantoin:- Know your ancestry.
- Ask if you’ve ever been tested for G6PD deficiency.
- Don’t assume you’re safe just because you’ve taken it before.
- Request a safer alternative if you’re unsure.
Can nitrofurantoin cause hemolytic anemia even if I’ve taken it before without problems?
Yes. G6PD deficiency doesn’t always cause symptoms unless triggered. You might have taken nitrofurantoin before and felt fine, but your enzyme levels can fluctuate. Factors like illness, stress, or even certain foods can lower your G6PD activity temporarily. If your body was under stress the first time you took it, you might have escaped hemolysis. The next time, under different conditions, your red blood cells might not survive the oxidative stress. Never assume past tolerance means future safety.
Is G6PD testing covered by insurance?
In the U.S., Medicare and most private insurers cover G6PD testing if ordered by a physician for clinical reasons, like before prescribing oxidant drugs. The test typically costs $35-$50 with Medicare reimbursement. However, some insurers require pre-authorization, and some clinics don’t bill for it directly. If you’re unsure, ask your provider to check your coverage before ordering the test.
What are the signs of hemolytic anemia from nitrofurantoin?
Symptoms usually appear within 1-3 days of starting the drug. Watch for: dark or tea-colored urine, sudden fatigue, yellowing of the skin or eyes (jaundice), rapid heartbeat, shortness of breath, fever, or dizziness. Lab tests will show low hemoglobin, high bilirubin, low haptoglobin, and high reticulocyte count. If you’re taking nitrofurantoin and notice any of these, stop the drug and seek medical help immediately.
Can I take nitrofurantoin if I have a mild case of G6PD deficiency?
The CPIC guidelines recommend avoiding nitrofurantoin entirely in all patients with G6PD deficiency, regardless of severity. Even mild deficiency can lead to acute hemolysis under oxidative stress. There’s no reliable way to predict how your body will react. The risk isn’t worth it when safer alternatives like fosfomycin are available. Don’t gamble with your red blood cells.
Should I get tested for G6PD deficiency if I’m planning to get pregnant?
Yes-if you’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent. G6PD deficiency is inherited, and if you’re a carrier, your baby could inherit it too. Nitrofurantoin is commonly prescribed during pregnancy for UTIs. If you’re deficient and take it, your baby could develop neonatal jaundice or hemolytic anemia from drug exposure in utero or through breast milk. Testing before pregnancy or early in prenatal care can prevent serious complications.
Why isn’t nitrofurantoin banned if it’s so dangerous?
It’s not banned because it’s still effective and safe for the majority of people-about 95% of users. The risk is real but concentrated in specific populations. Banning it would deprive millions of a low-cost, low-resistance antibiotic for UTIs. Instead, regulators focus on warnings and education. The goal isn’t to remove the drug, but to make sure it’s only used where it’s safe. The challenge is getting that message to every doctor and patient.

11 Comments
January 5, 2026 josh plum
Let me get this straight - doctors are just throwing nitrofurantoin at women like it’s candy, but if you’re Black? Suddenly you need a blood test? This isn’t medicine, it’s systemic neglect dressed up as protocol. I’ve seen this exact pattern with diabetes, hypertension, you name it. They don’t care until someone dies. And then they act shocked. Wake up, America - your healthcare system is rigged.
And don’t even get me started on how ‘G6PD deficiency is rare’ is the lie they tell to avoid doing the work. 400 million people worldwide. That’s not rare. That’s a global epidemic they’re ignoring because it’s cheaper to bury bodies than fix systems.
January 6, 2026 John Ross
From a pharmacogenomics standpoint, this is a textbook case of pharmacokinetic vulnerability. Nitrofurantoin is a nitrofuran derivative that generates reactive oxygen species (ROS) via redox cycling, overwhelming the NADPH-dependent glutathione reductase pathway in G6PD-deficient erythrocytes. The enzyme deficiency results in insufficient NADPH production, which compromises the cell’s ability to maintain reduced glutathione - the primary intracellular antioxidant.
What’s concerning is the clinical inertia. Even with CPIC and FDA Class C warnings, EHR systems lack decision support alerts. No CPT code integration. No automated flagging. It’s not negligence - it’s structural. We need CDS rules tied to ancestry flags and prior drug exposure history. Until then, this is preventable iatrogenic harm on an industrial scale.
January 8, 2026 saurabh singh
Bro, I’m from India and my cousin got hospitalized after taking nitrofurantoin for a UTI. We didn’t even know about G6PD deficiency until then. My grandma had it too - she always said her urine turned dark after eating fava beans. Turns out, that’s a classic trigger.
But here’s the thing - in India, we get tested for this as kids. It’s part of routine newborn screening in some states. Why is the US still playing Russian roulette with antibiotics? Get the $40 test. It’s cheaper than your next ER visit. And if you’re a doc - stop being lazy. One quick finger prick saves lives.
January 8, 2026 Dee Humprey
I’m a nurse and I’ve seen this too many times. A 28-year-old woman comes in with a UTI, gets nitrofurantoin, leaves, and two days later she’s back in the ER pale as a ghost, jaundiced, barely breathing. She didn’t know she had G6PD deficiency. No one asked. No one checked.
Just ask. One question. ‘Have you ever had dark urine after illness or been told you have anemia?’ That’s it. It takes 10 seconds. Don’t wait for a death to make you care.
January 8, 2026 Jay Tejada
So let me get this straight - you’re telling me the same drug that’s fine for your white neighbor is gonna kill me because I’m brown? And we’re supposed to be grateful it’s ‘only’ $50 to test for it? Meanwhile, my insurance denies it unless I’ve already turned blue.
Man, this isn’t science. It’s racism with a stethoscope.
January 10, 2026 Allen Ye
The real tragedy here isn’t the drug - it’s the epistemological failure of modern medicine. We have the tools to prevent this: genomics, point-of-care diagnostics, pharmacovigilance databases. Yet we persist in treating patients as statistical aggregates rather than biological individuals.
This isn’t about nitrofurantoin. It’s about the commodification of health. We’ve outsourced care to efficiency metrics and cost-per-case algorithms. We’ve forgotten that medicine is a moral practice, not a logistics problem.
When a system prioritizes speed over safety, it doesn’t just make mistakes - it kills. And then it calls those deaths ‘rare adverse events’ while the families pick up the pieces.
Maybe the question isn’t ‘why aren’t we testing?’ - but ‘why do we still think this is acceptable?’
January 10, 2026 mark etang
It is imperative to underscore that the administration of nitrofurantoin in individuals with glucose-6-phosphate dehydrogenase deficiency constitutes a contraindicated therapeutic intervention per current clinical guidelines issued by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Food and Drug Administration (FDA).
Therefore, it is the professional obligation of all prescribing clinicians to conduct pre-prescription screening for G6PD status, particularly in populations with known genetic prevalence. Failure to do so constitutes a deviation from the standard of care and exposes both patient and provider to significant legal and ethical liability.
Adoption of point-of-care testing protocols in primary care settings is not merely advisable - it is an ethical imperative.
January 11, 2026 Jason Stafford
THIS IS A BILLION-DOLLAR COVER-UP. Big Pharma knows nitrofurantoin kills people with G6PD deficiency. They’ve known for decades. But they don’t want to pay for testing. They don’t want to lose sales. So they bury the data, silence the doctors, and push the blame onto ‘unlucky patients.’
And now they’re pushing ‘fosfomycin’ as the ‘safe’ alternative? Funny how that’s only available in Europe. Coincidence? I think not.
Someone’s getting rich off dead people. And the FDA? They’re just the janitors cleaning up the blood.
WHO IS PROFITING FROM THIS? I’m not just asking - I’m demanding answers.
January 13, 2026 Mandy Kowitz
Oh my god I’m so tired of this. I got nitrofurantoin last year, felt fine, and now I’m supposed to panic because I’m ‘at risk’? I’m a 30-year-old woman who’s never had jaundice. Why do I need to be punished for my ancestry? This isn’t medicine - it’s guilt-tripping with a lab report.
Also, why are all the commenters suddenly experts? Did we all get a memo? ‘Today’s topic: G6PD Deficiency and the Moral Responsibility of Antibiotics.’
Just give me the pill. I’ll take my chances.
January 13, 2026 Justin Lowans
There’s a quiet revolution happening in primary care - one that’s slow, underfunded, and mostly invisible. Clinics in Detroit, Atlanta, and even rural Kansas are starting to implement routine G6PD screening before prescribing oxidant antibiotics. Not because it’s trendy. But because their patients keep showing up in crisis.
The cost? $35 per test. The benefit? Lives saved, ER visits avoided, trust rebuilt.
This isn’t about politics or profit. It’s about doing the right thing - even when no one’s watching. And if your clinic isn’t doing this yet? Maybe it’s time to ask why.
January 13, 2026 josh plum
And now the author replies like a saint - ‘ask your doctor.’ Like that’s gonna happen. My doctor doesn’t even know what G6PD stands for. He just hits ‘nitrofurantoin’ in the dropdown and moves on.
So yeah, I’ll ask. And he’ll say, ‘You’re fine.’ And I’ll take the pill. And maybe next time, I won’t be so lucky.
Thanks for the advice, doc. Really.
Write a comment