What CPAP and BiPAP Actually Do
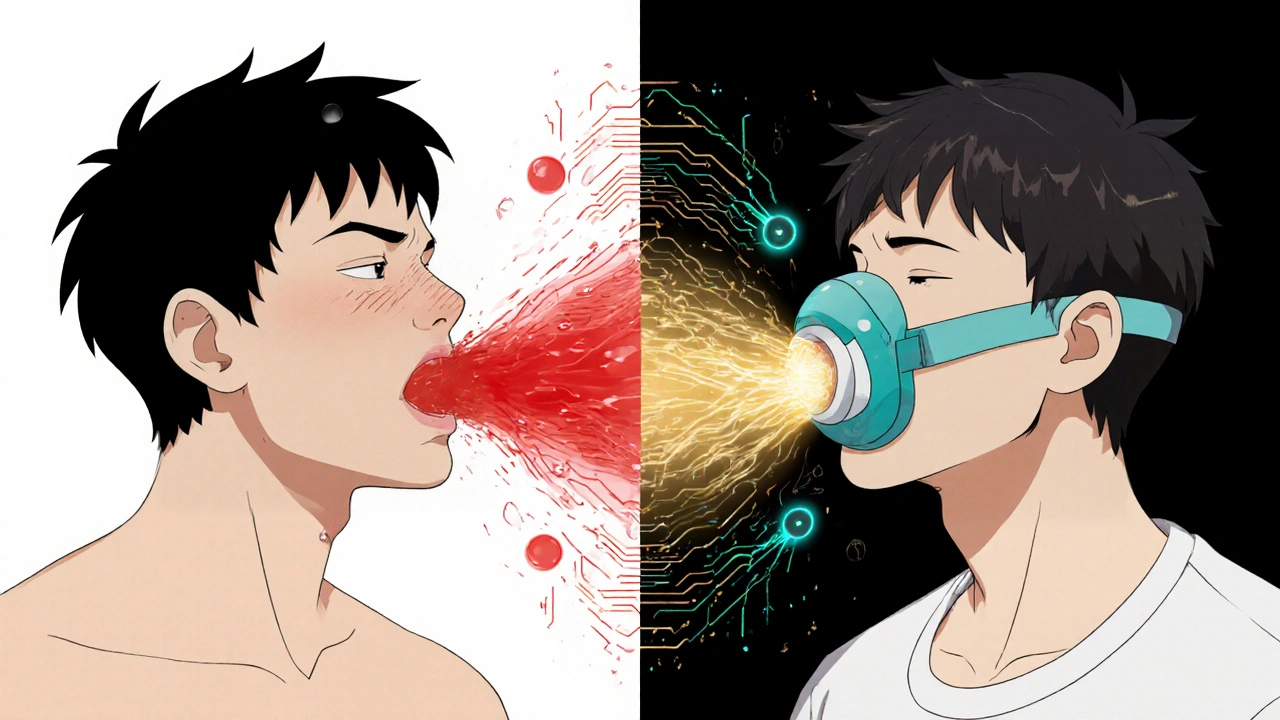
Both CPAP and BiPAP machines help you breathe better while you sleep. They push air through a mask to keep your airway open, stopping snoring and pauses in breathing. This is especially important if you have obstructive sleep apnea - where your throat muscles relax too much and block your airway. The main difference isn’t in how they treat sleep apnea, but in how they deliver air.
CPAP gives you one steady pressure all night. Whether you’re breathing in or out, the air pressure stays the same. BiPAP gives you two different pressures: a higher one when you inhale (IPAP), and a lower one when you exhale (EPAP). This makes it easier to breathe out, especially if you’re used to high pressures or have other lung conditions.
How the Machines Work - Side by Side
Think of CPAP like holding a steady breeze against your face. It’s constant, simple, and works for most people with sleep apnea. BiPAP is more like a pump that pushes air in harder and lets it out gently - like a bellows instead of a steady wind.
CPAP machines typically run between 4 and 20 cm H₂O of pressure. Most people need between 8 and 12. BiPAP machines go higher: IPAP can reach up to 30 cm H₂O, while EPAP stays lower, usually between 4 and 25. The gap between the two pressures must be at least 3 cm H₂O for the machine to work properly. This difference is what makes BiPAP easier to tolerate for some users.
Modern BiPAP devices also have backup features. If you stop breathing for too long - common in central sleep apnea - the machine will force a breath. CPAP doesn’t do this. It only keeps your airway open. It doesn’t breathe for you.
Who Gets CPAP - and Who Gets BiPAP
Eight out of ten people with sleep apnea start with CPAP. It’s the gold standard. If your main problem is your airway collapsing during sleep, CPAP fixes it. It’s cheaper, simpler, and just as effective as BiPAP for pure obstructive sleep apnea.
BiPAP isn’t a better version of CPAP. It’s a different tool for different problems. You’re more likely to get BiPAP if:
- You need high pressure (above 15 cm H₂O) and can’t tolerate exhaling against it
- You have COPD and your blood still holds too much carbon dioxide (hypercapnia)
- You have central sleep apnea - where your brain forgets to tell your lungs to breathe
- You have obesity hypoventilation syndrome - where extra weight makes breathing hard even when awake
- You have a neuromuscular disease like ALS or muscular dystrophy
For example, someone with COPD and sleep apnea (called overlap syndrome) often needs BiPAP. Their lungs are already weak. CPAP pressure alone won’t help them clear CO₂. BiPAP’s higher inhale pressure pushes air in deeper, while the lower exhale pressure lets them breathe out without fighting the machine.
Cost, Insurance, and Real-World Prices
CPAP machines cost between $500 and $1,200. A basic ResMed AirSense 10 runs around $899. BiPAP machines start at $800 and can hit $1,800. The Philips DreamStation BiPAP Auto sells for about $1,499.
Insurance doesn’t treat them the same. Medicare and most private insurers will cover CPAP right away if your sleep study confirms sleep apnea. But for BiPAP? You usually need proof that CPAP didn’t work. That means you tried it for at least 30 days, used it over 4 hours a night, and still couldn’t tolerate the pressure - especially if it was over 15 cm H₂O.
That’s a big hurdle. Many people switch to BiPAP because CPAP felt like choking. But insurers won’t pay unless you document that failure. Some doctors skip this step and prescribe BiPAP upfront - but that can lead to denied claims and out-of-pocket costs.
Does BiPAP Help You Sleep Better? The Evidence
Here’s the surprise: BiPAP doesn’t make most people sleep better than CPAP - if they only have obstructive sleep apnea. A major 2021 Cochrane review of nearly 2,000 people found no meaningful difference in sleep quality, daytime tiredness, or how often people used their machine. CPAP users averaged 5.1 hours per night. BiPAP users? 5.2.
So why do people swear by BiPAP? Because it’s easier to breathe out. One Reddit user wrote: “BiPAP at 14/8 felt like breathing normally. CPAP at 14 felt like I was drowning.” That’s not about curing sleep apnea - it’s about comfort. And comfort leads to use. If you stop using your machine, it doesn’t matter how good it is.
For people with COPD or central apnea, BiPAP clearly helps. Studies show it reduces nighttime breathing effort by 30-40% compared to CPAP at the same pressure. That’s not a small win. It means less strain on the heart, better oxygen levels, and fewer hospital visits.
What Users Really Say - The Good, the Bad, and the Ugly
On CPAP.com’s 2023 survey of over 12,000 users, 78% were happy with CPAP. About 62% used it 6+ hours a night. For BiPAP users, satisfaction was lower at 72%, but usage was higher - 68% used it 6+ hours. Why? Because they had no choice. Their bodies needed the two-pressure system.
But BiPAP isn’t easy to use. One in three BiPAP users said they struggled with settings. Machine cycling - when the device doesn’t sync with your breath - was a complaint from 27%. That feels like gasping or fighting the machine. CPAP users rarely report this. It’s simpler. Less to go wrong.
CPAP wins on ease. 71% rated it as “excellent” for ease of use. Only 58% said the same for BiPAP. Setup is faster. Troubleshooting is easier. Most people learn CPAP on their own using online videos. BiPAP often needs a respiratory therapist to fine-tune it.
What Happens After You Start
Both machines need time to get used to. Most people need 2 to 4 weeks to feel normal with CPAP. With BiPAP? 3 to 6 weeks. Why longer? More settings. More variables. More chances for things to feel off.
Insurance companies require you to use your machine at least 4 hours a night, 70% of nights, for the first 3 months. If you don’t meet that, they’ll stop paying. About 65% of CPAP users hit that mark. BiPAP users? 60%. That’s not because BiPAP doesn’t work - it’s because it’s harder to master. If your mask leaks, your pressure feels wrong, or your machine cycles poorly, you’re more likely to give up.
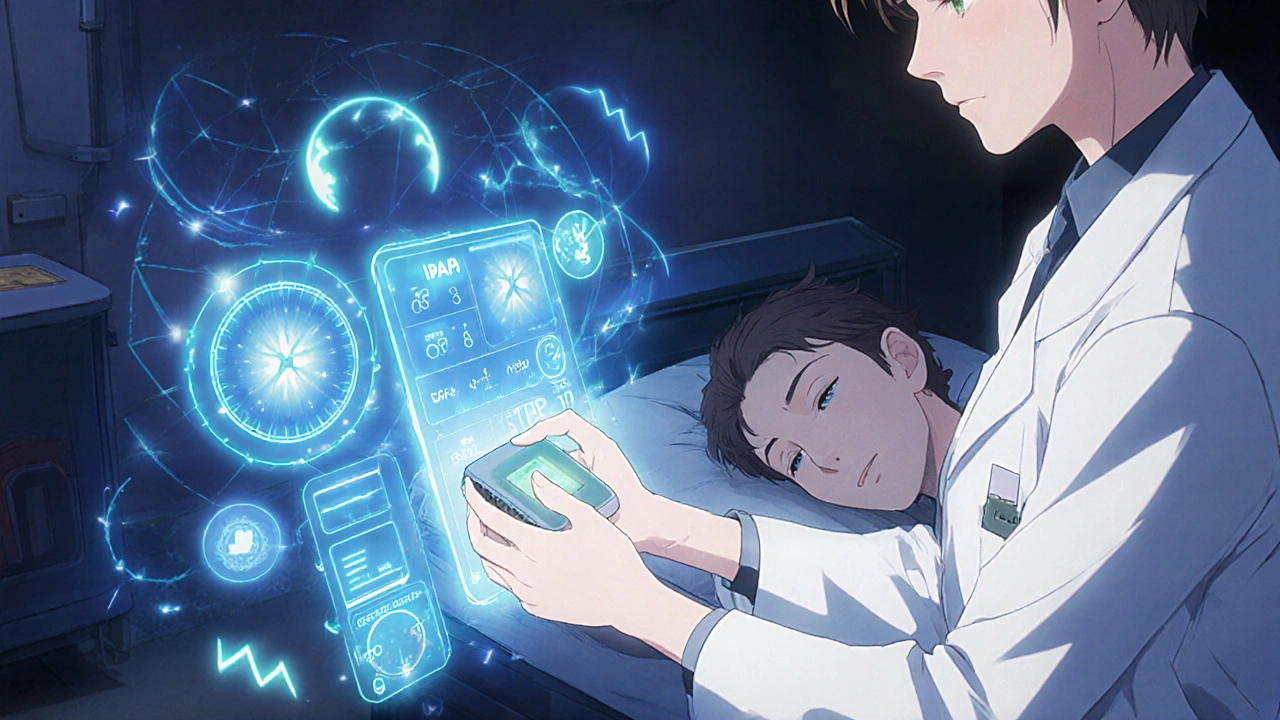
That’s why professional help matters. A good sleep clinic won’t just hand you a machine. They’ll check your mask fit, adjust humidity, and teach you how to clean it. For BiPAP, they’ll make sure the backup rate and pressure settings match your breathing pattern. One bad setting can ruin your whole night.
What’s New in 2025
Manufacturers are making smarter machines. ResMed’s AirCurve 10 VAuto now uses AI to adjust pressure on the fly - reading your breaths and changing IPAP and EPAP automatically. Philips’ DreamStation 3 includes built-in oxygen sensors to track your blood oxygen levels while you sleep.
These aren’t just gimmicks. They help doctors adjust therapy without another sleep study. But they’re expensive. And insurance doesn’t always cover them. The real innovation isn’t in the tech - it’s in making these machines easier to live with. Less noise. Lighter masks. Better data.
Still, the core truth hasn’t changed: CPAP works for most. BiPAP saves lives for a few. The goal isn’t to pick the fanciest machine. It’s to pick the one you’ll actually use.
What to Do Next
If you’ve been diagnosed with sleep apnea, start with CPAP. It’s the standard for a reason. Give it a real shot - at least 30 days. Use it every night. Adjust your mask. Try different humidifier settings. Talk to your sleep tech. Many people quit too soon because they didn’t fix the small things.
If CPAP feels unbearable - especially if you’re gasping on exhale, or your pressure is above 15 - ask your doctor about BiPAP. Don’t assume it’s a downgrade. It’s not. It’s the right tool for a different problem.
And if you have COPD, heart failure, or neurological issues? Make sure your sleep specialist knows. That changes everything. BiPAP isn’t just for sleep apnea. It’s for people whose bodies need extra help breathing - day and night.
Is BiPAP better than CPAP for sleep apnea?
No, not for most people. CPAP is just as effective at keeping your airway open. BiPAP is only better if you can’t tolerate CPAP pressure, have central sleep apnea, COPD, or another condition that makes breathing hard. For simple obstructive sleep apnea, BiPAP doesn’t improve outcomes - it just makes exhaling easier.
Can I switch from CPAP to BiPAP on my own?
No. You can’t just change the settings. BiPAP requires a new sleep study to set both IPAP and EPAP correctly. Your doctor needs to prescribe it based on your breathing patterns. Trying to adjust it yourself can make your sleep worse or even be dangerous if you have underlying lung disease.
Why does my BiPAP machine feel like it’s fighting me?
That’s usually a timing issue. The machine’s breath detection isn’t syncing with your breathing. This happens if the sensitivity is set too high or too low, or if your mask leaks. It can also occur if your EPAP is too close to your IPAP - the pressure difference needs to be at least 3 cm H₂O. Talk to your sleep therapist to recalibrate the machine.
Does insurance cover BiPAP if CPAP didn’t work?
Yes - but only if you prove CPAP failed. Most insurers require you to use CPAP for 30 days, at least 4 hours a night, and still have trouble tolerating the pressure - especially above 15 cm H₂O. Your doctor must document this. Without proof, insurance will deny the claim, and you’ll pay out of pocket.
Can I use a BiPAP machine if I don’t have sleep apnea?
Only under medical supervision. BiPAP is a medical device. It’s not meant for general use. People with COPD, heart failure, or neuromuscular diseases may need it even without sleep apnea. But using it without a diagnosis can lower your blood pressure too much, cause dizziness, or disrupt your natural breathing rhythm. Never use one without a doctor’s order.


14 Comments
November 22, 2025 Pramod Kumar
Been using a BiPAP for 3 years now after my COPD diagnosis. CPAP felt like a brick on my chest. BiPAP? It’s like my lungs finally got a break. The exhale pressure is a game-changer. No more waking up gasping like a fish out of water.
November 23, 2025 Richard Wöhrl
Important note: if you're on BiPAP and your machine feels like it's fighting you, check the trigger sensitivity AND your mask seal. I had a 2cm H₂O gap between IPAP/EPAP and kept thinking the machine was broken - turns out, my mask was leaking 12% of the time. Fixed it, and now I sleep like a baby. Also, humidity settings matter more than people admit.
November 24, 2025 Laurie Sala
Why do people act like BiPAP is some magical cure? I tried it. It’s just more expensive and more complicated. My CPAP worked fine. They just want to sell you a $1500 machine so they can make more money. I’m not falling for it.
November 25, 2025 Suresh Ramaiyan
There’s a quiet truth here: it’s not about which machine is better - it’s about which one lets you sleep. I’ve seen patients with ALS who couldn’t even lift their heads, and BiPAP gave them 5 extra hours of restful breathing. That’s not a gadget. That’s dignity. CPAP is for the majority. BiPAP is for the ones who need more than just an airway - they need a partner in breathing.
November 27, 2025 Adrian Rios
Let’s be real - insurance is the real villain here. I had to fight for 8 months to get BiPAP approved. I used CPAP for 45 days, logged every hour, sent my sleep data in triplicate, and still got denied because the doc didn’t check the ‘failed tolerance’ box correctly. Meanwhile, my wife’s cousin got BiPAP on the first try because he had a neurologist who knew how to write the note. This isn’t medicine. It’s bureaucracy with a stethoscope.
And don’t get me started on how clinics just hand you a machine and say ‘good luck.’ No one teaches you how to clean the tubing properly. I had mold growing in my hose because no one told me to rinse it daily. That’s negligence disguised as care.
Also - the AI-adjusting machines? They’re cool, but they’re not magic. I had one that kept thinking I was breathing faster than I was and kept boosting pressure. Woke me up every 20 minutes. Had to reset it manually. Tech is great until it’s working against you.
Bottom line: if you’re struggling with CPAP, don’t give up. Try new masks, humidifiers, chin straps. But if you’re still gasping on exhale? Push for BiPAP. Don’t wait for insurance to say yes. Get a second opinion. Your lungs don’t care about paperwork.
November 28, 2025 Matthew Mahar
BiPAP at 16/8 felt like breathing for the first time in 10 years. CPAP at 16 felt like trying to suck air through a straw taped to my face. I cried the first night I used it. Not from sadness - from relief. Why is this not common knowledge??
November 30, 2025 shreyas yashas
India here. We don’t have insurance, so we pay out of pocket. My dad’s BiPAP cost me 2 months’ salary. But he sleeps 7 hours now. Used to wake up 5 times a night. Machine is noisy, but worth it. CPAP? He hated it. Said it felt like a dragon sitting on his chest. BiPAP? He calls it his ‘quiet dragon’ now.
November 30, 2025 Lisa Detanna
As someone who’s tried both, I’ll say this: comfort > efficacy. CPAP fixes the apnea. BiPAP fixes the suffering. If you’re not using your machine, it doesn’t matter how perfect it is. I switched to BiPAP because I was quitting CPAP. Now I use it 7+ hours. That’s the win.
December 2, 2025 Javier Rain
Biggest myth: BiPAP is only for severe cases. I had mild OSA but high pressure needs (18 cm H₂O). CPAP felt like a tire pump on my face. BiPAP at 18/12? Smooth. No choking. No panic. I didn’t need COPD or ALS to benefit. Just needed to exhale without screaming.
Doctors act like BiPAP is a last resort. It’s not. It’s a tool. Use the right tool for the job.
December 3, 2025 Casper van Hoof
The philosophical underpinning of this entire debate rests on a simple axiom: human beings are not machines, yet we are treated as if we are. CPAP assumes uniformity; BiPAP acknowledges variability. The former seeks to enforce a solution; the latter adapts to the individual. In this light, BiPAP is not merely a medical device - it is an act of epistemological humility.
December 3, 2025 Kane Ren
Just started CPAP last week. First night was rough. Second night? Better. Third? I slept through the whole thing. Don’t give up too fast. Mask fit matters more than pressure. And drink water. Dry mouth is the worst.
December 4, 2025 Demi-Louise Brown
For those considering BiPAP: consult a sleep specialist who understands respiratory physiology. Do not rely on online forums or anecdotal evidence alone. The settings require clinical calibration. Your health is not a trial-and-error experiment.
December 5, 2025 John Mackaill
My wife has ALS. She’s been on BiPAP for 18 months. The backup rate feature? It saved her life twice during the night. CPAP wouldn’t have done that. It’s not about comfort - it’s about survival. If you think BiPAP is overkill, you haven’t held someone’s hand while they struggle to breathe.
December 7, 2025 Brandy Walley
LMAO at all these people acting like BiPAP is some miracle device. I used it for 2 weeks and hated it. Too many settings. Too loud. My CPAP was fine. You just need to stop complaining and get used to it. Also, your mask is probably too tight. Stop squeezing your face like you’re trying to kiss a cactus.
Write a comment