DOACs: What They Are, How They Work, and What You Need to Know
When you hear DOACs, Direct Oral Anticoagulants are a group of modern blood-thinning medications that prevent dangerous clots without needing regular blood tests. Also known as novel oral anticoagulants, they’ve changed how millions manage atrial fibrillation, deep vein thrombosis, and pulmonary embolism. Unlike older drugs like warfarin, DOACs work fast, don’t need constant monitoring, and have fewer food or drug interactions—making them easier to use for most people.
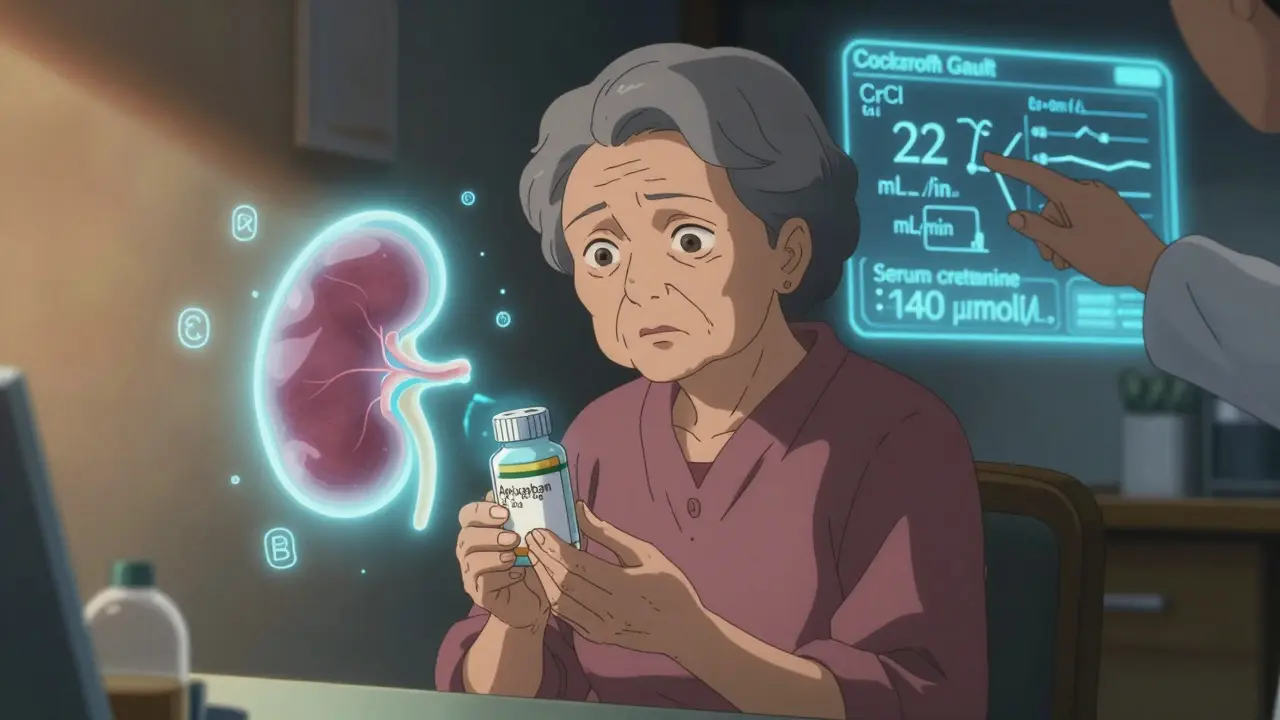
But they’re not magic. Warfarin, the long-standing anticoagulant that requires frequent INR checks and dietary restrictions. Also known as coumadin, it’s still used in specific cases like mechanical heart valves or severe kidney disease. DOACs include drugs like apixaban, rivaroxaban, dabigatran, and edoxaban—each with different dosing, half-lives, and how they’re cleared from the body. Some are safer for people with kidney issues, others work better for certain types of clots. You can’t just pick one based on price or convenience; your doctor needs to match the drug to your health profile.
And here’s what most people don’t realize: medication interactions, common drugs like NSAIDs, certain antibiotics, or even St. John’s Wort can make DOACs too strong or too weak. Also known as drug-drug interactions, these can lead to bleeding or clotting events that land you in the hospital. That’s why posts here cover real cases—like how a simple painkiller or a common antibiotic can turn a safe DOAC dose into a dangerous one. You’ll also find guides on managing side effects, knowing when to worry about bruising or blood in urine, and how to handle missed doses without panicking.
Older adults, especially those on multiple meds, are at higher risk for complications. That’s why you’ll see articles on fall risk, polypharmacy, and how DOACs fit into the bigger picture of senior medication safety. Some people take DOACs for stroke prevention while also using blood pressure pills, antidepressants, or heart rhythm drugs—each adding layers of complexity. The goal isn’t just to take the pill, but to understand how it fits into your whole health picture.
There’s no one-size-fits-all answer with DOACs. What works for a 65-year-old with atrial fibrillation might not be right for a 78-year-old with kidney trouble and a history of stomach bleeds. That’s why this collection gives you practical, no-fluff advice: how to talk to your doctor, what questions to ask, and how to spot warning signs before it’s too late. You’ll find comparisons, safety checklists, and real-world tips—not theory, not marketing.