DOAC Dosing Calculator for Renal Impairment
Patient Information
Important Notes
This tool calculates creatinine clearance using the Cockcroft-Gault formula, as recommended for DOAC dosing by the FDA, AHA, and ESC.
Always use CrCl (calculated with Cockcroft-Gault) instead of eGFR for DOAC dosing. eGFR overestimates kidney function in elderly patients.
Apixaban is generally the safest choice for renal impairment. The "ABC" rule applies: two or more of Age ≥80, Weight ≤60 kg, or Creatinine ≥1.5 mg/dL requires dose reduction.
Dosing Recommendations
When someone has atrial fibrillation and damaged kidneys, choosing the right blood thinner isn’t just about picking a pill-it’s about avoiding life-threatening mistakes. Direct Oral Anticoagulants (DOACs) like apixaban, rivaroxaban, dabigatran, and edoxaban replaced warfarin for most patients because they’re easier to use: no weekly blood tests, fewer food interactions, and more predictable effects. But when the kidneys aren’t working well, those same advantages turn into risks. Too much drug builds up. Too little leaves clots unchecked. And the difference between safety and disaster often comes down to one number: creatinine clearance.
Why Renal Impairment Changes Everything
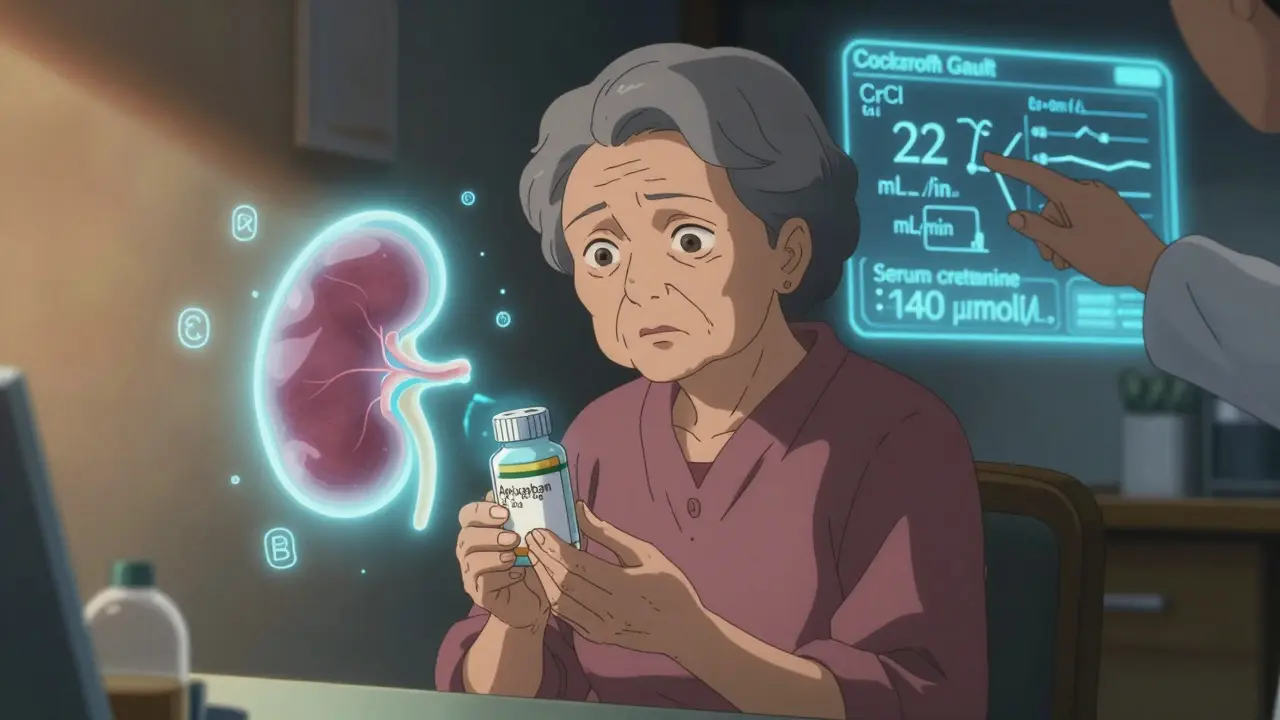
DOACs don’t all work the same way in the body. About 25% to 35% of each drug is cleared by the kidneys. For someone with healthy kidneys, that’s fine. But if your kidneys are struggling-say, with a creatinine clearance below 30 mL/min-those drugs stick around longer. That means higher blood levels. Higher levels mean higher bleeding risk. In fact, studies show that nearly half of all patients on DOACs for atrial fibrillation also have some degree of kidney disease. And in those patients, improper dosing is the leading cause of serious bleeding events.The problem isn’t just about how much drug is given. It’s about how we measure kidney function. Many doctors use eGFR from lab reports. But that’s wrong. For DOACs, you must use the Cockcroft-Gault formula to calculate creatinine clearance (CrCl). Why? Because eGFR was designed for general kidney disease tracking, not drug dosing. The FDA, the American Heart Association, and the European Society of Cardiology all say: use CrCl. Not eGFR. Not serum creatinine alone. The Cockcroft-Gault equation factors in age, sex, weight, and serum creatinine. For older, thinner patients-especially women over 80-it often gives a lower number than eGFR. And that lower number might be the one that saves their life.
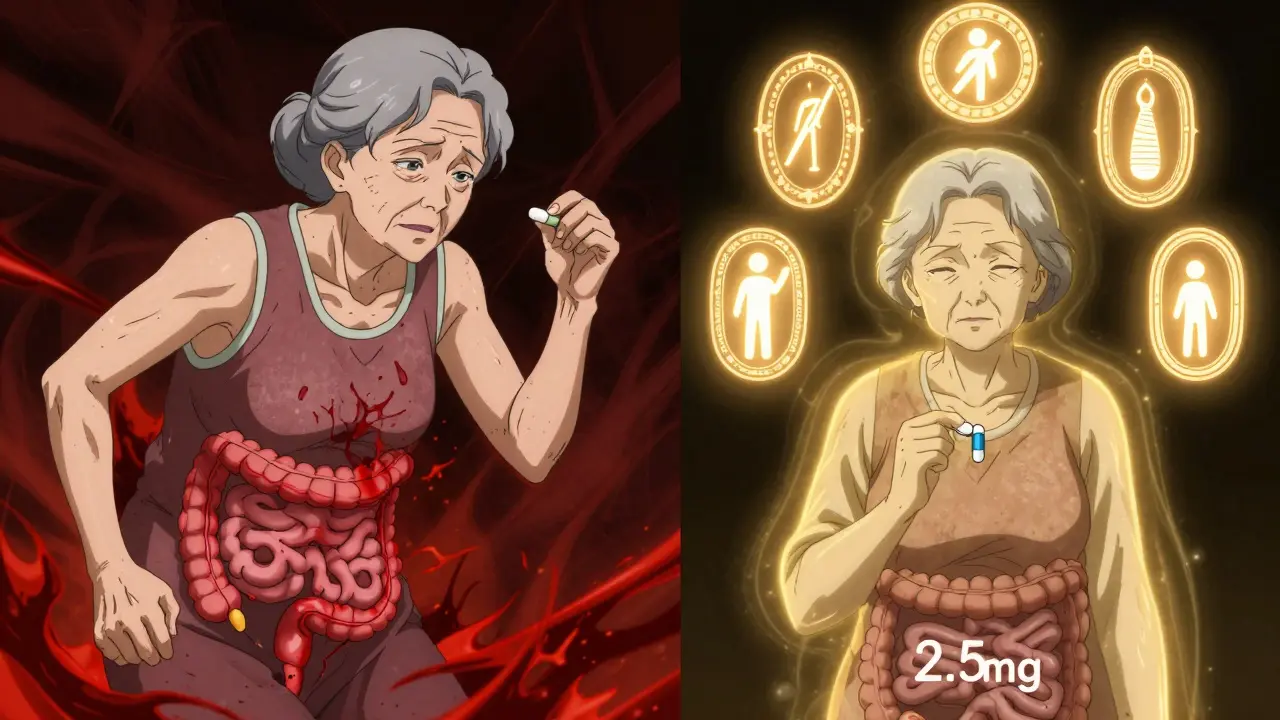
Apixaban: The Safest Choice for Kidneys
Among all DOACs, apixaban stands out. It’s the only one with data showing it can be used-even in patients on dialysis-with less bleeding than warfarin. The FDA label doesn’t require a dose change just because of kidney function alone. But that doesn’t mean you give everyone the full dose. The real rule for apixaban is this: reduce it to 2.5 mg twice daily if the patient meets at least two of these three criteria:- Age 80 or older
- Body weight 60 kg (132 lbs) or less
- Serum creatinine 133 μmol/L (1.5 mg/dL) or higher
That’s it. No need to check CrCl if you know those three things. But if CrCl is below 15 mL/min, don’t use apixaban at all. Even though some studies show it’s used safely in dialysis patients, official guidelines still say it’s contraindicated. Still, real-world data from nephrology clinics tell a different story. One UK-based team reported 127 dialysis patients on apixaban 2.5 mg twice daily with a major bleeding rate of just 1.8% over 18 months-far lower than their warfarin group’s 3.7%. That’s why many cardiologists now consider apixaban the go-to for advanced kidney disease.
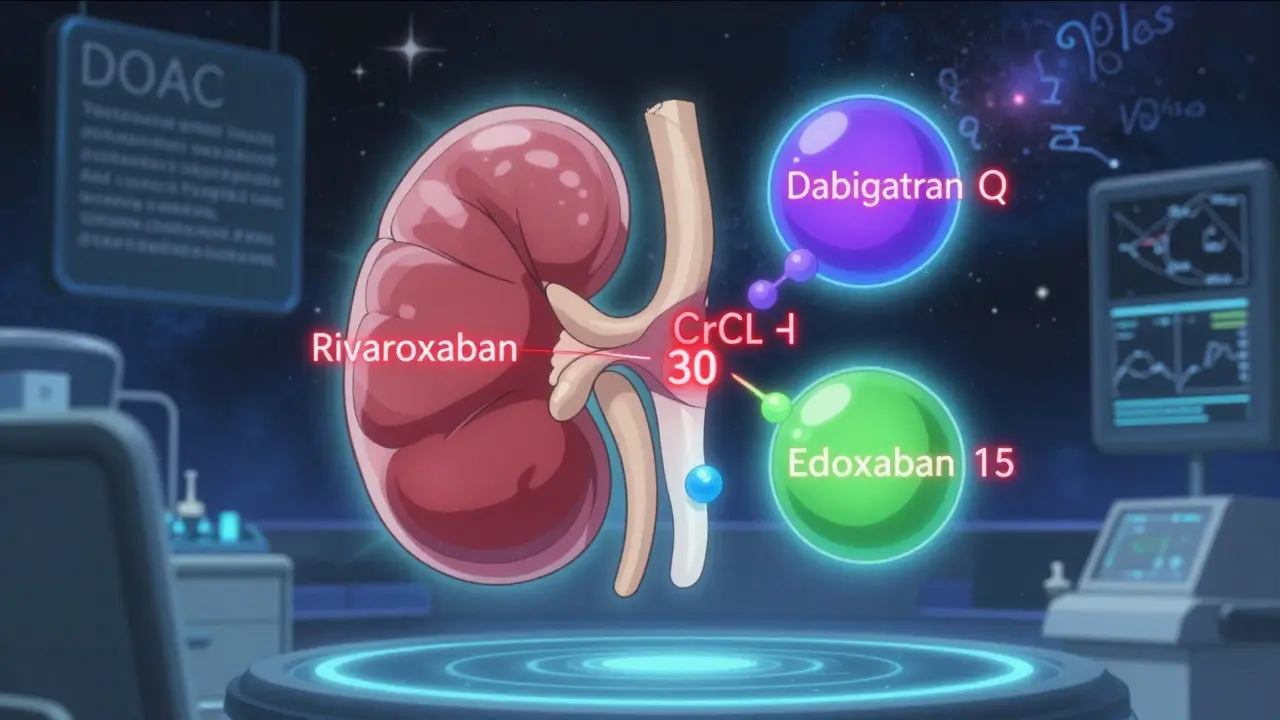
Rivaroxaban and Dabigatran: Use With Caution
Rivaroxaban is off-limits if CrCl is below 15 mL/min. Period. Even if the patient seems stable, the risk of bleeding skyrockets. It’s not worth the gamble. Dabigatran follows the same rule: no use below CrCl 15 mL/min. For CrCl between 15 and 30 mL/min, reduce the dose to 75 mg twice daily. But here’s the catch: dabigatran has a higher bleeding risk than apixaban in this group. A 2020 study found that in patients with CrCl between 15 and 30 mL/min, dabigatran led to 40% more major bleeds than apixaban. That’s not a small difference. It’s enough to change practice.Both drugs are also more affected by drug interactions. Dabigatran is cleared partly through gut transporters, so common medications like verapamil or rifampin can spike its levels. Rivaroxaban interacts with strong CYP3A4 inhibitors like ketoconazole or clarithromycin. If a patient is on any of these, even a normal dose can become dangerous. That’s why many pharmacists now check for interactions before filling a DOAC prescription-especially in older patients on multiple meds.
Edoxaban: Narrow Window, Narrower Margin
Edoxaban is the most sensitive to kidney function. If CrCl is between 15 and 50 mL/min, the dose drops to 30 mg once daily. Above 50, it’s 60 mg. Below 15? Not approved. And here’s the kicker: edoxaban’s effectiveness drops in moderate kidney disease. The ENGAGE AF-TIMI 48 trial showed that while it worked well in patients with normal kidneys, its ability to prevent strokes fell sharply in those with CrCl under 50 mL/min. So if you’re choosing between edoxaban and apixaban for someone with CrCl of 35 mL/min, apixaban is the better bet-not just because of safety, but because it actually works better in this group.The Real-World Mistakes Doctors Make
A 2022 study in JAMA Internal Medicine looked at over 12,000 DOAC prescriptions in patients with kidney disease. Nearly 37% had dosing errors. Most common? Giving the full dose to someone with CrCl under 30. Or worse-using eGFR instead of CrCl. One case in Bristol involved a 78-year-old woman with weight 52 kg and creatinine 140 μmol/L. Her eGFR was 38 mL/min, so her doctor prescribed 5 mg apixaban twice daily. But her CrCl? Just 22 mL/min. She was on the wrong dose. Three weeks later, she had a major gastrointestinal bleed. She survived, but barely. That’s not rare. It’s predictable.Another big mistake? Assuming all elderly patients are the same. A 2022 study in the American Journal of Health-System Pharmacy found that 28.4% of CrCl calculations in patients over 80 were inaccurate because they didn’t account for low muscle mass. Older adults, especially women, lose muscle as they age. Their creatinine drops-not because kidneys are better, but because muscle is gone. If you plug that low creatinine into the formula without adjusting for body size, you’ll overestimate kidney function. And that means too high a dose.
What to Do in Practice
Here’s how to get it right:- Calculate CrCl using Cockcroft-Gault-not eGFR. Use this formula:
(140 - age) × weight (kg) × (0.85 if female) / (72 × serum creatinine) - For apixaban: Use 5 mg twice daily only if CrCl > 30 mL/min AND no two of the three risk factors (age ≥80, weight ≤60 kg, creatinine ≥133 μmol/L). Otherwise, use 2.5 mg twice daily.
- For rivaroxaban: Only if CrCl ≥ 30 mL/min. Never use if CrCl < 15 mL/min.
- For dabigatran: Only if CrCl ≥ 30 mL/min. Reduce to 75 mg twice daily if CrCl 15-30 mL/min. Avoid below 15.
- For edoxaban: Reduce to 30 mg daily if CrCl 15-50 mL/min. Avoid below 15.
- Check kidney function at least once a year-and more often if the patient is unstable, on diuretics, or has an acute illness.
- Use the ABCs mnemonic for apixaban: Age, Body weight, Creatinine. Two out of three? Reduce the dose.
And if the patient is on dialysis? Apixaban 2.5 mg twice daily is the only option with real-world support. Even though it’s technically off-label, it’s the safest choice we have. Warfarin? It’s still used, but studies show it causes more brain bleeds and calcified blood vessels in dialysis patients. DOACs aren’t perfect-but in advanced kidney disease, apixaban is the least bad option.
What’s Coming Next
The AXIOS trial, though stopped early, is releasing data in late 2024 that could change guidelines. It looked at apixaban versus warfarin in dialysis patients. Early results suggest apixaban is not only safer-it may be more effective. Meanwhile, the RENAL-AF trial is comparing apixaban to adjusted warfarin in severe kidney disease. Results are expected in 2025. By 2026, we may finally have clear, evidence-based dosing for every stage of kidney failure. Until then, stick to the data we have: use apixaban, calculate CrCl, and never guess.Can I use eGFR to adjust DOAC doses in kidney disease?
No. eGFR is not accurate enough for DOAC dosing. Always use the Cockcroft-Gault formula to calculate creatinine clearance (CrCl). Guidelines from the FDA, AHA, and ESC all specify CrCl as the standard. Using eGFR can lead to overdosing and serious bleeding.
Is apixaban safe for patients on dialysis?
Yes, apixaban 2.5 mg twice daily is the most commonly used and safest DOAC in dialysis patients. While not officially approved for this group, real-world data from nephrology clinics show lower bleeding rates compared to warfarin. Other DOACs like rivaroxaban and dabigatran are not recommended. Always use the reduced dose, even if the patient seems healthy.
Why is body weight important for apixaban dosing?
Low body weight (≤60 kg) means less volume to distribute the drug, leading to higher blood concentrations. When combined with age ≥80 or high creatinine, it signals reduced clearance. Meeting two of these three factors triggers a dose reduction to 2.5 mg twice daily-even if CrCl is above 30 mL/min. This is a key safety rule often missed in practice.
Can I switch from warfarin to a DOAC if the patient has kidney disease?
Yes-if CrCl is above 30 mL/min, DOACs are preferred over warfarin. They’re safer and more effective. If CrCl is between 15 and 30 mL/min, apixaban is the best choice. Below 15 mL/min, apixaban 2.5 mg twice daily is still the most evidence-backed option. Warfarin increases risk of brain bleeds and vascular calcification in advanced kidney disease.
How often should I check kidney function in someone on a DOAC?
At least once a year. But if the patient is over 75, has diabetes, is on diuretics, or has recently had an infection or hospital stay, check every 3-6 months. Kidney function can drop quickly in older adults. A sudden rise in creatinine could mean your patient is now on too high a dose.

14 Comments
February 11, 2026 Karianne Jackson
So basically if your grandma is tiny and old and her kidneys are junk, just give her half the pill and pray? 😅 I mean, I get it, but this feels like playing Russian roulette with blood thinners. My aunt almost died from this exact thing. Never again.
February 11, 2026 Tom Forwood
Bro this post is a lifesaver. I work in pharmacy and we get so many of these wrong. I once had a 81yo lady on 5mg apixaban because her eGFR was 38. Her CrCl was 19. She bled out through her gums for 3 days. We switched her to 2.5mg and she’s been fine for 2 years now. Use Cockcroft-Gault. Always. Stop using eGFR. It’s not even close.
February 12, 2026 John McDonald
Love this breakdown. Apixaban really is the MVP here. I’ve seen so many docs just default to rivaroxaban because it’s cheaper or they’re lazy. But in renal impairment? Nah. Apixaban’s the one that actually lets you sleep at night. Also, the ABCs mnemonic? Genius. I’m putting that on my whiteboard tomorrow.
February 13, 2026 Chelsea Cook
Ohhh so THAT’S why my 83yo patient kept getting bruised like a grape? I thought it was just ‘old lady skin.’ Turns out I was giving her full dose apixaban because her eGFR was ‘fine.’ My bad. Now I calculate CrCl like a boss. Also, low weight + age + high creatinine? Two out of three = reduce. I’m writing that on my hand.
February 15, 2026 Andy Cortez
Y’all are overcomplicating this. DOACs are a scam. Warfarin’s been around for 70 years. Why are we chasing shiny new pills that kill people? My cousin died on apixaban. They said ‘it’s safe’ - yeah right. The FDA’s in bed with Big Pharma. Check the trials - they excluded the sickest patients. Real people? We’re guinea pigs.
February 15, 2026 Jacob den Hollander
Thank you for this. Seriously. I’m a nurse practitioner and I’ve been terrified of dosing DOACs in elderly patients. This gives me clarity. The Cockcroft-Gault point? Game changer. I just started using it last month and already caught two wrong doses. One was a 79yo woman on 5mg - CrCl was 18. She’s now on 2.5mg and hasn’t had a bleed. Thank you for saving lives with clear info.
February 15, 2026 Patrick Jarillon
They’re all lies. The ‘guidelines’? Written by pharma reps in Cancún. CrCl? A myth. Real kidney function is measured by urine output, not math formulas. And dialysis? They’re lying when they say apixaban works. My uncle was on it for 6 months - then his legs turned black. They said ‘it’s normal.’ I know what they’re hiding. They don’t want you to know about the 2018 leaked study. Google ‘RENAL-AF suppression.’
February 15, 2026 Randy Harkins
This is so helpful 💙 I’ve been nervous about switching my dad from warfarin because of his kidney numbers. Now I feel confident. Apixaban 2.5mg it is. Also, the ABCs trick? I’m sharing this with my whole family. Thank you for making something scary feel manageable. You’re a real one 🙌
February 16, 2026 Chima Ifeanyi
From a nephrologist in Lagos: The Cockcroft-Gault equation is obsolete. It’s based on Caucasian male muscle mass. In African populations, especially with high prevalence of sarcopenia, it underestimates CrCl by 20–30%. We use adjusted formulas - or better yet, cystatin C. Your entire algorithm is flawed. This is why we have 4x higher bleeding rates in our cohort. Fix your bias.
February 17, 2026 Jonah Mann
Wait wait wait - so if someone’s 79, weighs 58kg, and has creatinine of 1.6 - you reduce apixaban even if CrCl is 35? I thought the rule was CrCl <30? This changes everything. I’ve been giving full doses to 3 people. Oh god. I’m calling them right now. Thank you. Seriously. This could’ve killed someone.
February 18, 2026 THANGAVEL PARASAKTHI
Bro I’m from Tamil Nadu and we have so many elderly patients with low muscle mass. We used to use eGFR. Now we use Cockcroft-Gault with weight correction. One lady, 82, 48kg, creatinine 1.2 - eGFR was 40, CrCl was 21. We reduced her dose. No bleed in 14 months. This post? Saved lives. Thank you.
February 20, 2026 Frank Baumann
Let me tell you about the time I had a patient on rivaroxaban with CrCl 14. I didn’t catch it because the EHR auto-filled eGFR. He had a subdural hemorrhage. He’s now in a nursing home. I’ve been fired. My license is suspended. I’ve been to therapy. I’ve written 17 letters of apology. I’ve read every guideline. I’ve cried in the shower. I’ve changed my life. Don’t let this happen to you. CrCl. Not eGFR. Always. Always. Always. I’m not okay. But you can be.
February 20, 2026 Chelsea Deflyss
Wow. Just… wow. I’m a nurse and I’ve been doing this wrong for years. I thought if the patient was stable, the dose was fine. I didn’t know about the ABCs. I didn’t know weight mattered. I didn’t know CrCl was different from eGFR. I’m embarrassed. I’m changing my practice today. I’m so sorry to every patient I’ve hurt.
February 21, 2026 Tricia O'Sullivan
Thank you for this meticulously detailed and evidence-based exposition. The clarity with which you have delineated the renal pharmacokinetics of DOACs, particularly the nuanced distinctions between Cockcroft-Gault and eGFR, is both academically rigorous and clinically indispensable. I shall certainly integrate these recommendations into my institutional protocols with immediate effect.
Write a comment