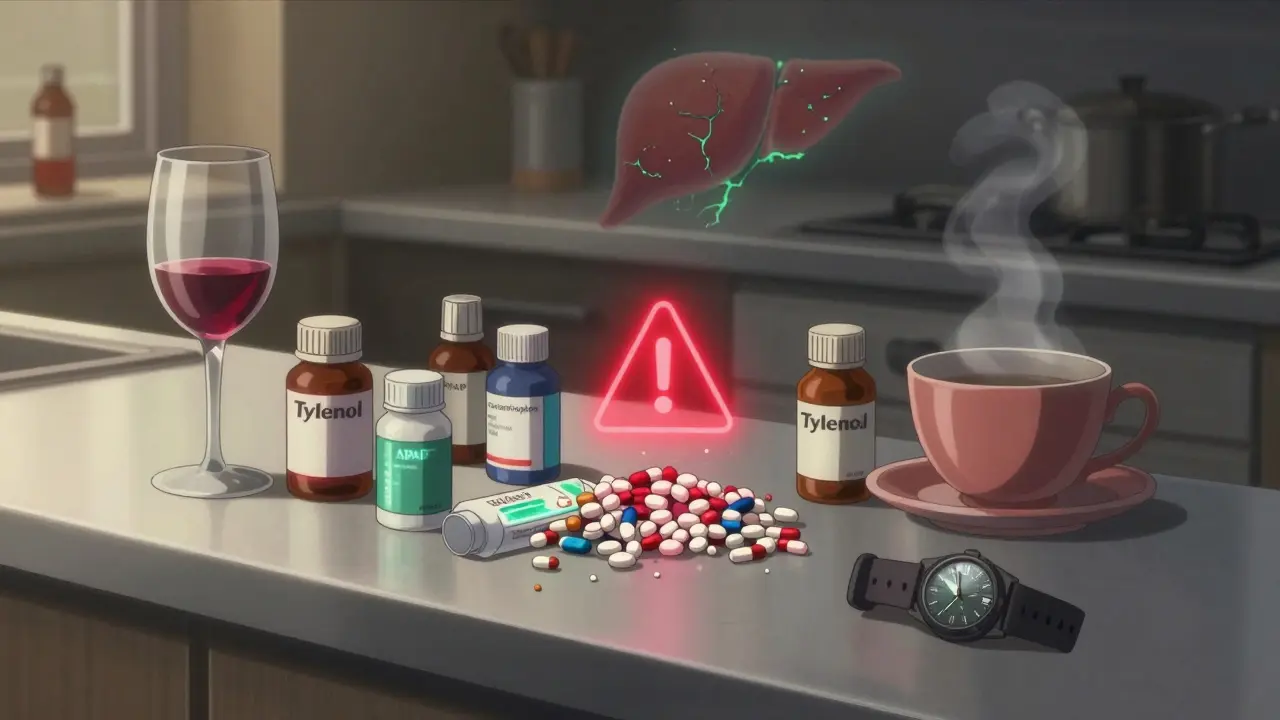
Acetaminophen is in almost every medicine cabinet in the UK and the US. You know it as Tylenol, Panadol, or just the little white pill you reach for when your head hurts or you have a fever. It’s safe-if you use it right. But here’s the thing: acetaminophen is also the leading cause of acute liver failure in the United States, and it’s happening to people who never meant to overdose. They just didn’t realize how easy it is to go over the limit.
How Much Is Too Much?
The maximum safe daily dose for adults is 4,000 milligrams. That’s eight 500mg tablets. Sounds simple, right? But most people don’t know that acetaminophen hides in dozens of other medications. Cold and flu remedies, sleep aids, prescription painkillers like Vicodin and Percocet-they all contain it. You take one for your headache, another for your stuffy nose, and a third for your sleep. Suddenly, you’ve taken 6,000 mg without ever thinking about it.
And it’s not just about taking too many pills at once. Chronic overuse-taking 3,000 mg or more every day for weeks-can also damage your liver. That’s because your liver can only process so much acetaminophen at a time. Once it hits its limit, it starts producing a toxic byproduct called NAPQI. Normally, your body neutralizes it with glutathione. But when you overload the system, glutathione runs out, and NAPQI starts eating away at your liver cells.
For kids, the limit is even tighter: 10-15 mg per kilogram of body weight per dose, no more than five doses in 24 hours. Never give a child adult-strength tablets. And never use a kitchen spoon to measure liquid medicine. A teaspoon isn’t the same as a tablespoon-and 41% of pediatric overdoses happen because of this mistake, according to JAMA Pediatrics.
The Silent Warning Signs
One of the most dangerous things about acetaminophen overdose is how quiet it is at first. You might feel fine for 12 to 24 hours after taking too much. No vomiting. No pain. Just a little nausea, maybe some sweating. That’s Stage I. By the time your stomach starts hurting, your liver is already under attack.
Stage II hits between 24 and 72 hours. That’s when the pain shows up-sharp, right under your ribs on the right side. You feel tired. Your skin might look yellow. Your urine turns dark. Blood tests will show liver enzymes spiking-sometimes over 10,000 IU/L. Normal is under 40. At this point, you’re in serious trouble.
Stage III, around days three to four, is when the body starts to shut down. Jaundice. Confusion. Bleeding gums. Kidneys fail. Half of the patients with full liver failure also develop kidney failure. If you’re not treated by now, your chances of survival drop fast.
And here’s the kicker: you don’t need to take a whole bottle to cause damage. Just 7.5 grams in one go-fifteen 500mg tablets-is enough to trigger acute liver failure in many adults. For someone with existing liver disease or who drinks alcohol regularly, the threshold is even lower.
Why Alcohol Makes It Worse
If you drink alcohol regularly-even just a glass or two a day-your liver is already working harder to break it down. That means it has less capacity to handle acetaminophen. Studies show that people who drink three or more alcoholic drinks daily have a much higher risk of liver damage from even therapeutic doses of acetaminophen.
It doesn’t matter if you had your drink the night before. Alcohol keeps your liver enzymes active for hours, making them more likely to produce toxic NAPQI when acetaminophen comes in. That’s why doctors tell you to avoid alcohol completely while taking acetaminophen. No exceptions.
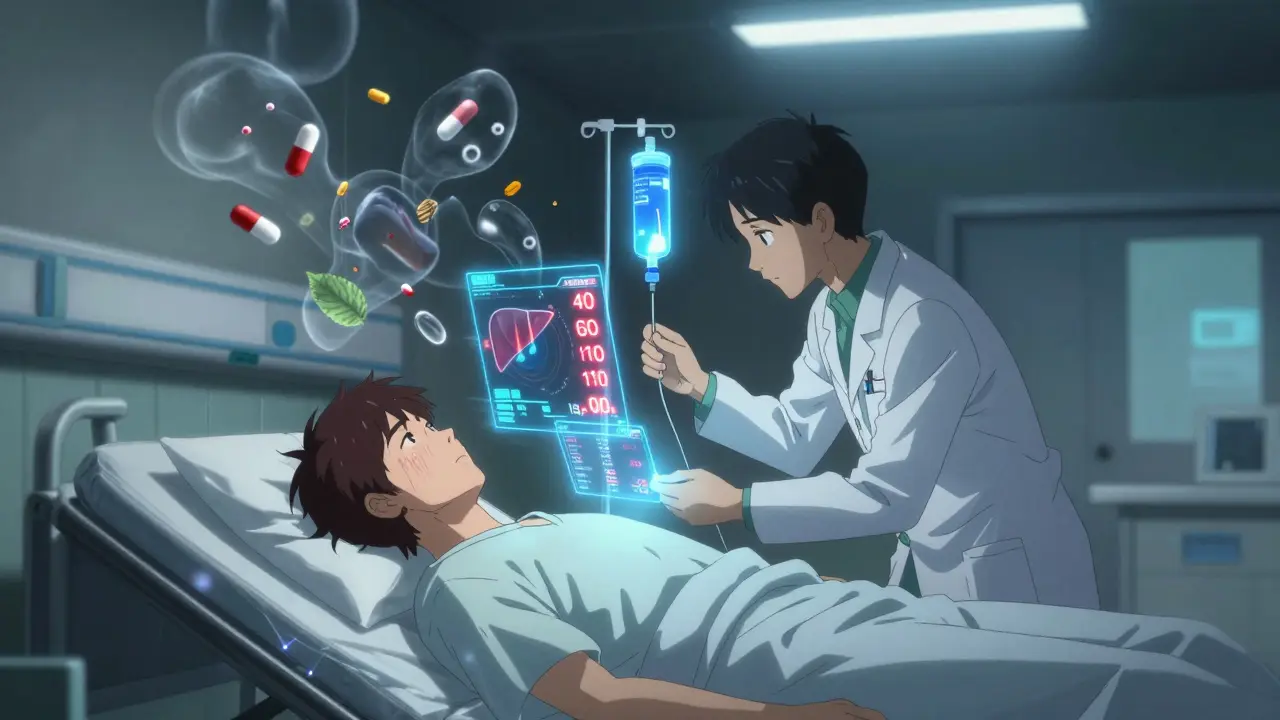
The Antidote That Saves Lives
There’s good news: there’s a highly effective antidote-N-acetylcysteine, or NAC. It works by replenishing glutathione, the body’s natural shield against NAPQI. But timing is everything. If you get NAC within 8 hours of an overdose, your chance of full recovery is over 90%. After 16 hours, that drops to 60%. After 24 hours? The damage is often irreversible.
That’s why calling Poison Control immediately is the most important thing you can do. Don’t wait for symptoms. Don’t hope it’ll pass. If you think you’ve taken too much-even if you feel fine-call now. In the U.S., it’s 1-800-222-1222. In the UK, dial 111 and ask for the Poisons Information Service. They’ll tell you what to do next.
How to Prevent an Accidental Overdose
Here’s what actually works to stay safe:
- Read every label. Look for “acetaminophen” or “APAP.” It’s not always obvious. Some brands hide it in tiny print. If you see it on two different pills, don’t take both.
- Set a daily cap. Never exceed 3,000 mg a day if you’re over 65, have liver disease, or drink alcohol. Even 4,000 mg is risky for some people.
- Use a pill tracker. Write down what you take and when. Use a notes app or a small notebook. It’s easy to forget how many you’ve already taken.
- Never mix with alcohol. Not even one drink. Not even on weekends.
- Use the right measuring tool. For kids, always use the syringe or cup that comes with the bottle. Never use a kitchen spoon.
- Ask your pharmacist. If you’re on multiple medications, ask them to check for hidden acetaminophen. They’re trained to spot this.
What the Labels Don’t Tell You
The FDA requires a liver warning on all acetaminophen products. But studies show only 38% of people actually understand what it means. The warning is small. The word “acetaminophen” is often printed in light gray. Meanwhile, the brand name-Tylenol, Panadol, Excedrin-is huge and bold.
That’s why so many people don’t realize they’re doubling up. They see “Tylenol” on one bottle and “Cold & Flu Relief” on another. They think they’re safe because they’re not taking “extra Tylenol.” But both have the same ingredient.
There’s a push right now to make “acetaminophen” appear in bold, larger font on all labels. But until that happens, you have to be the one watching out for it.
Who’s Most at Risk?
It’s not just people who try to “tough out” pain. The biggest group of accidental overdoses? Adults between 30 and 50. They’re taking painkillers for back pain, cold medicine for a cold, and sleep aids for insomnia-all on top of a glass of wine or two. They’re not trying to harm themselves. They just didn’t know the math added up.
Older adults are also at higher risk. Many take multiple prescriptions and don’t realize acetaminophen is in one of them. And people with chronic liver disease-like fatty liver or hepatitis-are more vulnerable, even at low doses. The American Association for the Study of Liver Diseases says these patients should never take more than 2,000 mg per day.
What to Do If You Think You’ve Overdosed
Don’t wait. Don’t Google it. Don’t hope it’ll go away.
Call your local poison control center immediately. If you’re in the UK, call 111. If you’re in the US, call 1-800-222-1222. Tell them exactly what you took, how much, and when. They’ll tell you whether you need to go to the ER.
If you’re in the ER, ask for NAC. Don’t accept just painkillers or IV fluids. NAC is the only thing that reverses the damage. And if you’re told you’re fine because you don’t “look sick,” get a second opinion. Liver damage doesn’t show up on the outside.
Recovery is possible-even after severe overdose-if treatment starts early. But every hour counts.
Final Thought: It’s Not About Fear. It’s About Awareness.
Acetaminophen isn’t evil. It’s one of the safest painkillers when used correctly. It doesn’t hurt your stomach like ibuprofen. It doesn’t raise your blood pressure like aspirin. But its safety is conditional. It only works if you respect the numbers.
So next time you reach for that bottle, pause. Read the label. Count the pills. Think about what else you’ve taken today. Your liver doesn’t scream before it breaks. It just… stops.
Can I take acetaminophen if I have a fatty liver?
Yes-but only at a reduced dose. If you have fatty liver disease, hepatitis, or any form of chronic liver damage, your doctor should limit your daily acetaminophen to no more than 2,000 mg. Even that should be used only when necessary. Your liver is already under stress, and acetaminophen adds to it. Always check with your doctor before using it regularly.
Is it safe to take acetaminophen while pregnant?
Acetaminophen is considered the safest pain reliever during pregnancy, and it’s commonly recommended by OB-GYNs for headaches, back pain, or fever. But it should still be used at the lowest effective dose for the shortest time possible. Avoid long-term daily use. Some recent studies suggest a possible link between very high or prolonged use and developmental issues in children, so don’t take it just because it’s “safe”-take it because you need it.
What’s the difference between Tylenol and regular acetaminophen?
None. Tylenol is a brand name for acetaminophen. The active ingredient is identical. Generic versions, store brands, and international names like Panadol all contain the same chemical. The only differences are price, inactive ingredients (like fillers), and packaging. Always check the label for “acetaminophen” or “APAP,” not the brand name.
Can I take acetaminophen with ibuprofen?
Yes, and many doctors recommend alternating them for better pain control. You can take 500 mg of acetaminophen and 400 mg of ibuprofen at the same time, as long as you don’t exceed the daily limit for either. But never take a combination product that already has both. That’s how accidental overdoses happen. Stick to single-ingredient pills and track each one separately.
How do I know if I’ve damaged my liver from acetaminophen?
You won’t feel it until it’s advanced. The only way to know is through blood tests. Liver enzymes (ALT and AST) rise before symptoms appear. If you’ve taken more than 4,000 mg in a day or have been taking it daily for weeks, ask your doctor for a liver panel. Don’t wait for yellow skin or pain. By then, it’s too late for prevention.
Are children’s acetaminophen products safer than adult ones?
Not inherently. The concentration is lower in children’s formulas, but that doesn’t mean they’re safer if misused. Giving a child an adult tablet-even half of one-can cause a dangerous overdose. Always use the dosing device that comes with the product. Never guess. And never use children’s syrup for an adult-it’s too weak and you’ll end up taking too much volume.

13 Comments
January 22, 2026 Ryan Riesterer
Acetaminophen metabolism is primarily mediated by CYP2E1 and UGT1A1 isoforms, with NAPQI formation being the rate-limiting step in hepatotoxicity. Glutathione depletion thresholds vary significantly based on genetic polymorphisms in GSTM1 and GSTT1. Chronic alcohol use induces CYP2E1 expression, lowering the toxic threshold by up to 40%. The 4,000 mg daily limit is a population-based approximation-individual pharmacokinetic variability demands personalized dosing, especially in hepatic impairment.
January 23, 2026 Patrick Roth
Let’s be real-this whole thing is a scare tactic pushed by Big Pharma so you’ll buy their ‘safer’ alternatives like ibuprofen, which actually causes more GI bleeds than acetaminophen causes liver failure. You’re more likely to die from a car crash on the way to the pharmacy than from a ‘toxic’ dose. Chill out. The real danger is people panicking over a drug that’s saved millions of lives.
January 24, 2026 Lauren Wall
Stop mixing meds. It’s not that hard. You’re not a chemist. Just read the label. One pill at a time. Done.
January 24, 2026 Tatiana Bandurina
Interesting how the FDA only mandated the warning after 2009, right after they approved that new combo drug with hydrocodone. Coincidence? Or did they know the risks all along and waited until they could profit from both the drug and the antidote? NAC is expensive, you know. And it’s not patented. Who benefits when you need emergency treatment? Think about it.
January 26, 2026 Philip House
Europe doesn’t have this problem. They regulate OTC meds like real medicines, not candy. In the UK, you can’t even buy more than 16 tablets without a pharmacist’s approval. Here? You walk into Walmart, grab three different bottles, and walk out with 2,000 mg of hidden acetaminophen in your cart. This isn’t freedom. It’s negligence dressed up as choice.
January 27, 2026 Akriti Jain
They’re hiding the truth. 🤫 The real reason they don’t ban acetaminophen is because the CDC uses liver failure stats to justify funding for ‘liver health programs’-which are just a front for vaccine trials. You think NAC is the antidote? Nah. It’s a placebo. The real cure is in the WHO’s secret database. They’re not telling you because they need you scared. 😈
January 27, 2026 Mike P
My uncle took 12 Tylenol for his back pain and thought he was fine. He woke up in the ICU three days later. Liver transplant. Now he’s on immunosuppressants. Don’t be that guy. Read the damn label. It’s not rocket science. And if you drink? Just don’t. Not even one beer. Your liver doesn’t care if it’s Friday night or not.
January 27, 2026 shivani acharya
Okay, so let’s break this down. You’re telling me that every single cold medicine, sleep aid, migraine pill, and ‘natural’ supplement in America has this poison hidden in it? And no one’s suing the manufacturers? And the FDA just sits there with their hands in their pockets while grandma takes three different bottles because they all say ‘relief’ on the front? This isn’t an accident. This is a corporate design. They want you to get sick. They want you to need NAC. They want you to need a liver transplant. Then you’re stuck in the system for life. And they profit from every step. It’s not a warning. It’s a trap. And you’re walking right into it. 😔
January 29, 2026 Sarvesh CK
While the pharmacological mechanisms of acetaminophen toxicity are well-documented, the broader societal implications warrant deeper reflection. The normalization of polypharmacy in modern healthcare reflects a systemic failure to prioritize patient education and medication reconciliation. The burden of vigilance is disproportionately placed on the individual, despite structural factors-such as fragmented prescribing, inconsistent labeling, and commercialized OTC marketing-that actively undermine safety. A truly preventive approach would require regulatory standardization, pharmacist-led medication reviews, and public health campaigns that treat pharmacokinetics as civic literacy, not personal responsibility.
January 29, 2026 Hilary Miller
My mom in Mumbai takes acetaminophen every day for arthritis. She never knew it was in the cold medicine she got from the local shop. No one here reads labels. We just trust the pharmacist. But now I’m teaching her to check for APAP. Small change, big difference.
January 29, 2026 Margaret Khaemba
I never realized how many products had acetaminophen until I started tracking my meds in a spreadsheet. I was taking 3,500 mg a day without knowing it. Now I only use single-ingredient pills and write down every dose. It’s annoying, but my liver thanked me.
January 31, 2026 Keith Helm
It is imperative that individuals exercising self-medication protocols adhere strictly to the maximum daily dosage thresholds delineated by regulatory authorities. Noncompliance constitutes a demonstrable failure of personal health stewardship.
February 1, 2026 Ryan Riesterer
Regarding the point on genetic variability: individuals homozygous for GSTM1-null genotype exhibit 30% lower glutathione conjugation capacity. This is clinically significant in chronic users. Genetic screening for GST polymorphisms should be considered in high-risk populations-especially those with chronic pain or alcohol use disorder. The one-size-fits-all 4,000 mg limit is outdated.
Write a comment