When your stomach hurts after eating, it’s easy to blame the food. But is it a food allergy or just a food intolerance? The difference isn’t just semantic-it changes everything about how you eat, live, and stay safe. One can send you to the ER in minutes. The other might just make you feel bloated for hours. And confusing them can lead to unnecessary fear, wrong diets, or even life-threatening mistakes.
What Happens in Your Body? Immune System vs. Digestive System
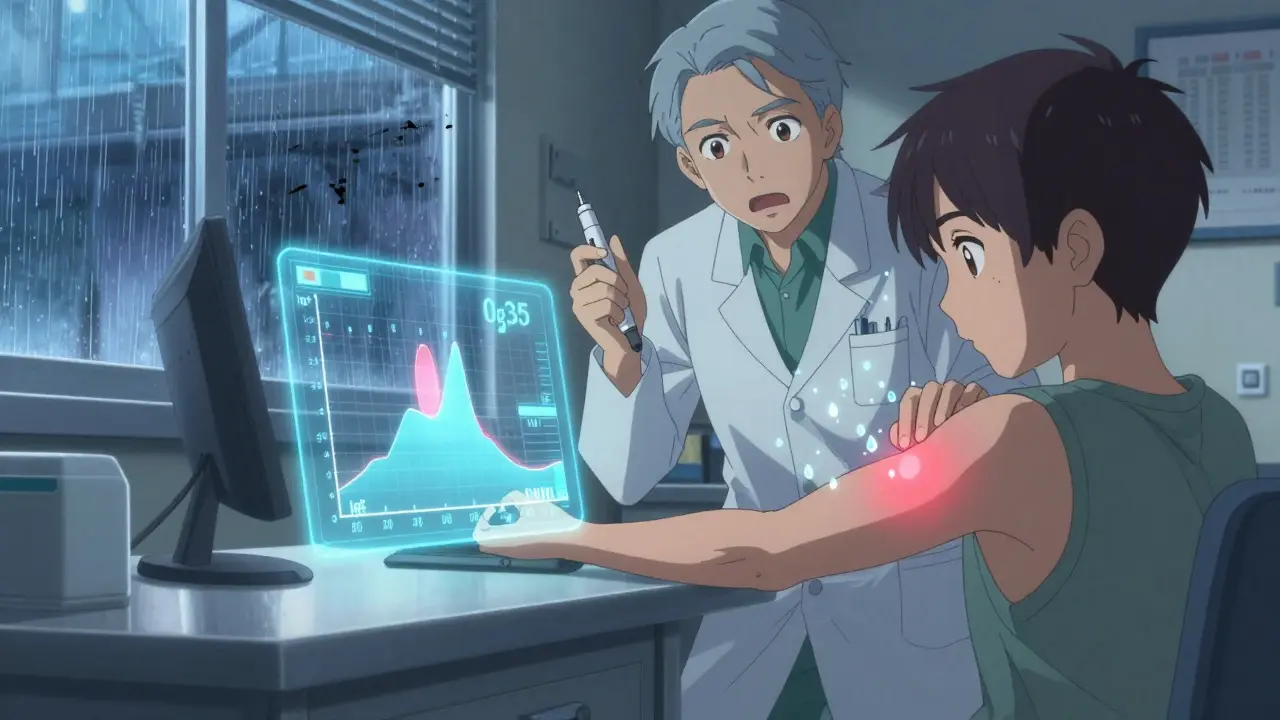
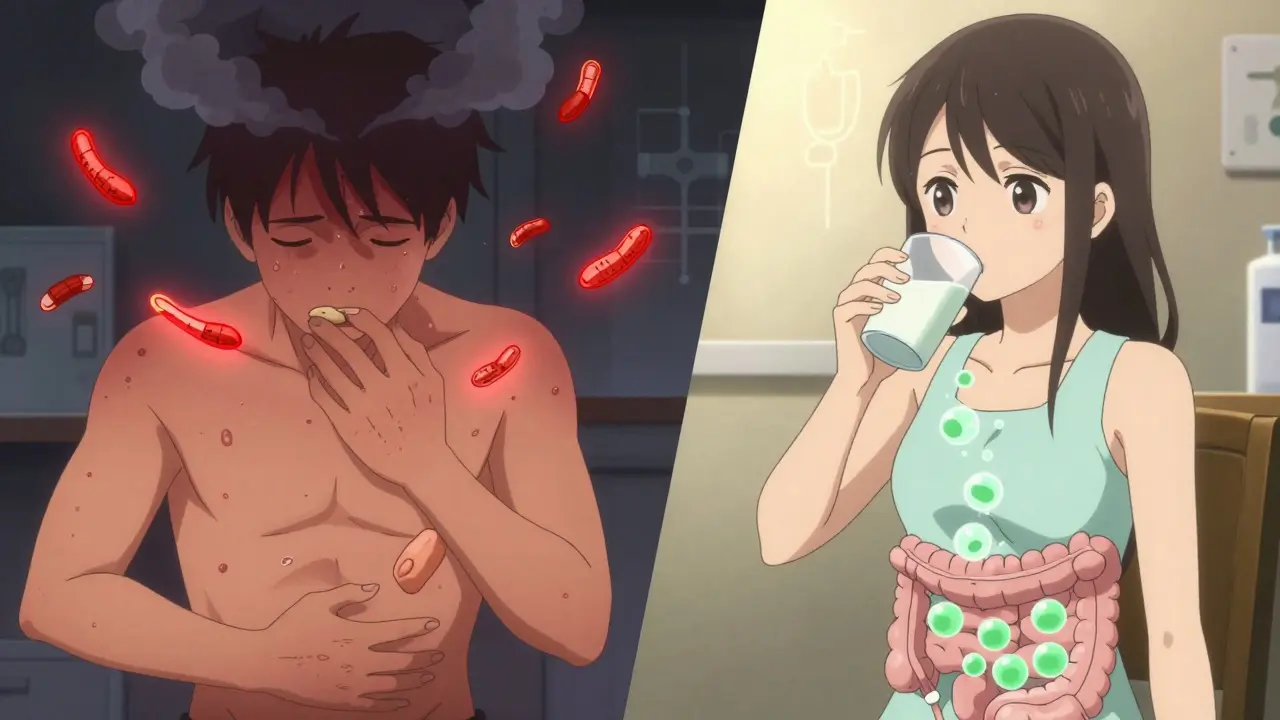
A food allergy is your immune system going into overdrive. It sees a harmless protein-like the one in peanuts or milk-as an invader. It produces IgE antibodies, which trigger mast cells to release histamine and other chemicals. That’s what causes hives, swelling, vomiting, or anaphylaxis. It happens fast: within minutes, sometimes seconds. Even a tiny crumb can set it off. Food intolerance is different. No immune system involved. No antibodies. Just your digestive system struggling to handle something. The most common cause? Enzyme deficiency. Lactose intolerance, for example, means your body doesn’t make enough lactase to break down milk sugar. So that sugar sits in your gut, gets fermented by bacteria, and produces gas, bloating, cramps, and diarrhea. Symptoms show up slower-usually 30 minutes to a few hours after eating. The key distinction? Food allergies can kill. Food intolerances won’t. That’s not just a slogan-it’s backed by clinical guidelines from the American Academy of Allergy, Asthma & Immunology. A 2023 study in JAMA Network Open confirmed that anaphylaxis from food allergies can start in under five minutes and requires epinephrine immediately. Food intolerance? It’s uncomfortable, maybe disruptive, but never life-threatening.GI Symptoms: How to Tell Them Apart
Both can cause stomach pain and diarrhea, but the pattern tells the story. If you have a food allergy, GI symptoms often come with other signs:- Sudden vomiting or diarrhea within minutes of eating
- Hives, itching, or swelling of lips/tongue
- Wheezing, coughing, or trouble breathing
- Dizziness or fainting
- Bloating and gas, usually starting 30 minutes to 2 hours after eating
- Cramping that comes and goes
- Diarrhea, but without systemic symptoms
- Nausea, sometimes
The Big Eight: What Foods Trigger Allergies?
Not all foods are equal when it comes to allergies. In the U.S., 90% of IgE-mediated reactions come from just eight foods, as defined by the FDA:- Peanuts
- Tree nuts (almonds, walnuts, cashews)
- Milk
- Eggs
- Wheat
- Soy
- Fish
- Shellfish
- Lactose (in dairy)
- FODMAPs (fermentable carbs in onions, garlic, beans, apples)
- Gluten (not always celiac-see below)
- Sulfites (in wine, dried fruit, processed meats)
- Fructose (in fruit, honey, high-fructose corn syrup)
Testing: What Works and What’s a Scam
If you suspect a food allergy, see an allergist. Don’t guess. Don’t rely on online tests. The gold standard for food allergy diagnosis is a three-step process:- Skin prick test: A tiny drop of allergen is placed on your skin, then lightly pricked. A wheal (raised bump) of 3mm or more compared to a control suggests allergy.
- Specific IgE blood test: Measures antibody levels in your blood. A result above 0.35 kU/L is considered positive-but false positives are common, especially in people with eczema.
- Oral food challenge: The only definitive test. You eat small, increasing amounts of the food under medical supervision. If you react, it’s confirmed. If not, it’s not an allergy.
- Hydrogen breath test: Used for lactose and fructose intolerance. You drink a sugar solution, then your breath is tested for hydrogen. A rise of 20 ppm above baseline confirms malabsorption.
- Celiac blood test: Looks for tissue transglutaminase IgA antibodies. Levels above 10 U/mL are highly suggestive. But you must be eating gluten at the time of the test-or you’ll get a false negative.
- Endoscopic biopsy: If celiac is suspected, a scope takes a sample of your small intestine. Marsh 3 classification means clear damage.
- Elimination and challenge diet: The go-to for non-celiac gluten sensitivity and FODMAP intolerances. Remove the suspect food for 2-6 weeks. Then reintroduce it. If symptoms return, it’s likely the culprit.
Managing Food Allergies: Strict Avoidance and Emergency Prep
If you have a food allergy, you need a plan.- Avoid the food completely. Even trace amounts can trigger a reaction.
- Read every label. The FDA’s 2021 FASTER Act requires clear labeling of the top nine allergens-even in restaurants.
- Carry two epinephrine auto-injectors (EpiPen or generic) at all times. They’re not optional. One might not be enough.
- Teach family, coworkers, teachers how to use them. Anaphylaxis doesn’t wait.
Managing Food Intolerances: Flexibility Over Fear
Food intolerances are about balance, not bans.- Lactose intolerance: Most people can handle up to 12 grams of lactose daily-about one cup of milk. Hard cheeses and yogurt often cause fewer issues because they’re lower in lactose.
- Non-celiac gluten sensitivity: Many find relief cutting out wheat and rye, but not necessarily all gluten. Oats (if pure) are often fine.
- FODMAPs: A low-FODMAP diet can help IBS symptoms. But it’s not meant to be lifelong. Reintroduction is key.
- Sulfites: Avoid wine, dried fruit, and processed meats if you react. Look for “contains sulfites” on labels.
Why Misdiagnosis Is Common-and Dangerous
A 2023 study in Clinical Gastroenterology and Hepatology found that 80% of people who think they have a food intolerance actually have something else:- 45% had IBS
- 12% had IBD (Crohn’s or ulcerative colitis)
- 23% had functional dyspepsia
What to Do Next
If you’re having regular GI symptoms after eating:- Track your food and symptoms in a journal. Note timing, portion size, and other factors.
- See a doctor. Don’t self-diagnose. Rule out celiac, IBD, or thyroid issues first.
- If allergy is suspected, see an allergist. Get skin or blood tests-and ask about an oral challenge.
- If intolerance is suspected, work with a dietitian. Start with an elimination diet under guidance.
- Avoid unproven IgG tests. They waste money and lead to unnecessary restrictions.
Can you outgrow a food allergy?
Yes, some children outgrow allergies to milk, eggs, wheat, and soy-often by age 10. Peanut, tree nut, fish, and shellfish allergies are less likely to be outgrown, but not impossible. Regular follow-up testing with an allergist is the only way to know.
Can you have both a food allergy and a food intolerance?
Absolutely. Someone might be allergic to peanuts and also intolerant to lactose. The two conditions don’t exclude each other. They just need different management strategies. One requires emergency epinephrine. The other might just need a lactose-free yogurt.
Is gluten intolerance the same as celiac disease?
No. Celiac disease is an autoimmune disorder where gluten damages the small intestine. Blood tests and biopsy confirm it. Non-celiac gluten sensitivity causes similar symptoms but no immune damage or antibodies. It’s diagnosed only after ruling out celiac and wheat allergy. Both need gluten avoidance, but only celiac carries long-term risks like osteoporosis or lymphoma if untreated.
Do food intolerances get worse over time?
Usually not. Lactose intolerance often increases with age because lactase production naturally declines. But other intolerances, like FODMAP sensitivity, don’t typically worsen unless you have an underlying condition like IBS or SIBO. Avoiding the food doesn’t make your body better at digesting it-you’re just avoiding the trigger.
Can stress make food intolerance symptoms worse?
Yes. Stress affects gut motility and sensitivity. People with IBS or functional gut disorders often notice worse symptoms during stressful periods. That doesn’t mean the food is the problem-it means your gut is more reactive. Managing stress with sleep, exercise, or therapy can help reduce flare-ups.
Are there any new tests coming for food intolerances?
Yes. Researchers are exploring metabolite biomarkers in blood to distinguish non-celiac gluten sensitivity from IBS. A 2024 Nature Communications study identified a pattern of 12 metabolites that correctly classified patients with 89% accuracy. These tests aren’t available yet, but they’re the future of personalized diagnosis.

13 Comments
December 31, 2025 Aaron Bales
Had a kid with a peanut allergy. Learned the hard way: one crumb = ER trip. Epinephrine isn't optional-it's life insurance. Always carry two.
Also, stop trusting those IgG tests. They're scams dressed up as science.
January 1, 2026 Sara Stinnett
Oh please. You're just feeding the medical-industrial complex with your rigid binaries. Allergy? Intolerance? Who even defines these categories anymore? The body doesn't care about your FDA charts.
It's all a spectrum of suffering, and your 'gold standard' tests are just glorified guesswork wrapped in white coats.
And don't get me started on 'oral challenges'-you're basically asking someone to nearly die for a diagnosis.
Maybe the real issue is that we've outsourced intuition to laboratories.
Our ancestors didn't need IgE titers to know if something disagreed with them.
They just... felt it.
Now we're medicated, tested, and utterly disconnected from our own biology.
What a sad, over-medicalized existence we've engineered.
At least the body still remembers what the lab forgot.
January 2, 2026 linda permata sari
OMG I JUST REALIZED I’M A LACTOSE HERO 🥹
Drank a whole glass of milk at 3 a.m. after a breakup… and lived to tell the tale! 🤪
But my belly? It screamed like a banshee. 😭
Now I sip almond milk like it’s liquid peace.
Also, I cried during the celiac part. This article got me.
Thank you for writing this like a love letter to gut health 💖
January 2, 2026 Brandon Boyd
Biggest takeaway? You don’t have to live in fear-but you DO need to be smart.
Track your meals. Talk to a dietitian. Don’t self-diagnose like it’s a TikTok trend.
And if you think gluten is the villain… maybe it’s not.
Try the low-FODMAP reset first. It’s life-changing for so many.
You’re not broken. You’re just misinformed.
And hey-you can still eat joyfully. Just smarter.
One bite at a time.
January 4, 2026 Branden Temew
So we’ve reduced the complexity of human digestion to a checklist of eight allergens and a few FODMAPs?
How poetic.
Our ancestors survived on fermented grains, raw milk, and wild game without a single IgE test.
And now we’re terrified of bread because a lab said so.
Who’s really allergic to food-or are we just allergic to uncertainty?
Maybe the problem isn’t what we eat…
but how much we’ve stopped listening to our bodies.
And yes, I’m aware this is the third time I’ve said ‘maybe’ in one comment.
It’s because I’m not sure anymore.
Neither is the medical system.
January 4, 2026 Frank SSS
Okay but like… why does everyone act like food allergies are some rare tragedy?
I’ve seen people freak out over trace nuts while chowing down on 30g of sugar and 500mg of sodium.
Meanwhile, I’ve got a cousin who’s lactose intolerant and eats cheese like it’s a religious ritual.
He’s fine. So maybe the whole thing’s just… stress?
Or maybe we’re just too lazy to cook real food.
Also, epinephrine costs what now? Who’s got that kind of cash?
Also also, I’m not even sure I believe in gluten sensitivity.
It’s just IBS with a fancy label.
January 4, 2026 Paul Huppert
Just wanted to say thanks for laying this out so clearly.
I’ve been confused for years about whether my bloating after pizza is allergy or intolerance.
Now I know to talk to an allergist before cutting out wheat.
Also, I didn’t realize IgG tests were useless.
Wasted $200 on one last year. Oof.
Appreciate the no-nonsense breakdown.
January 6, 2026 Hanna Spittel
ALERT: Big Pharma is using your stomach pain to sell EpiPens 💉💰
Also, the FDA? Controlled by corporations. Don’t trust their ‘top 8’ list.
They want you scared. So you buy their tests. Their meds. Their ‘gluten-free’ snacks at $12 a loaf.
Meanwhile, your grandma ate sourdough and lived to 98.
Wake up.
Also, I think my cat is allergic to my aura. 🐱👁️🗨️
January 8, 2026 Brady K.
Let’s be real-the entire food intolerance industrial complex is built on the myth that ‘you’re broken.’
‘Elimination diet’? Sounds like a cult.
‘Low-FODMAP’? More like ‘low-fun.’
And don’t even get me started on ‘component-resolved diagnostics’-it’s just jargon with a PhD.
Meanwhile, your microbiome is doing backflips while you’re obsessing over whether your yogurt has 0.1g of lactose.
Here’s the real diagnosis: you’re overthinking your dinner.
Go eat a burger. Don’t check the label.
Live a little.
Or don’t. I’m not your mom.
January 9, 2026 Kayla Kliphardt
I’ve had symptoms for years but never knew how to start. This helped me know what questions to ask my doctor.
Thank you for not making me feel crazy.
Just… one thing: can you recommend a good dietitian who gets this stuff?
I’m scared to go to the wrong one.
January 9, 2026 John Chapman
YES YES YES this is the most accurate thing I’ve read all year 🙌
My cousin had anaphylaxis at a birthday party-no one knew what to do.
Now I carry two EpiPens in my purse. Always.
Also, I switched to oat milk and my gut thanked me.
And no-I don’t care if it’s ‘not natural.’ I’m alive and not in pain.
That’s the win.
Let people live.
And if you’re reading this and scared? You got this. 💪❤️
January 11, 2026 Urvi Patel
Everyone is so obsessed with labels but no one knows what they are talking about. Lactose intolerance is just a modern myth created by dairy companies to sell lactase pills. The real issue is processed food. End of story.
January 11, 2026 anggit marga
In Nigeria we just eat and see what happens. If you get sick you drink ginger tea. If you die then you were not meant to live. Why do you Americans make everything a science project? This article is too long. I read 3 sentences and got bored.
Write a comment