HP Trigger Identifier
Is Your Environment Triggering Hypersensitivity Pneumonitis?
This tool helps identify potential triggers based on your living environment and symptoms. Remember: HP is caused by breathing in environmental antigens (like bird proteins or mold), not medications.
When you start coughing and feel short of breath, it’s easy to blame a cold, allergies, or even a new medication. But if these symptoms keep coming back-especially after being around birds, moldy hay, or humidifiers-you might be dealing with something more specific: hypersensitivity pneumonitis. And here’s the catch: it’s not caused by pills you swallow. It’s caused by what you breathe.
What Hypersensitivity Pneumonitis Really Is
Hypersensitivity pneumonitis (HP), sometimes called extrinsic allergic alveolitis, isn’t an infection or an allergy like asthma. It’s an immune reaction in the tiny air sacs of your lungs-the alveoli-triggered by repeated breathing in of certain airborne particles. These aren’t chemicals you take orally. They’re things you inhale: bird droppings, mold from damp hay, fungi in humidifiers, or dust from hot tubs. This condition doesn’t happen after one exposure. It takes repeated contact over weeks or months. Your immune system gets sensitized. Then, every time you breathe in the same dust or particles, your lungs swell up. That’s when coughing and breathlessness start. The Merck Manual and other top medical sources make this clear: HP is caused by environmental antigens, not medications. If you’re thinking your new blood pressure pill or antibiotic caused your lung symptoms, you’re likely looking at a different problem-like drug-induced interstitial lung disease. That’s not HP. It’s a different disease with different causes and different lung damage.How Cough and Breathlessness Show Up
The symptoms of HP don’t come on like a flu. They creep in, or they hit hard and fast-depending on how often you’re exposed. In the acute form, you might feel fine in the morning, then by late afternoon, you’re sweating, shivering, coughing, and struggling to catch your breath. It usually starts 4 to 8 hours after breathing in a big dose of the trigger-like cleaning out a bird cage or walking through a moldy barn. If you get away from the source, you often feel better within a day or two. The subacute form is sneakier. You don’t have a fever or chills. Instead, you just feel tired. Your cough sticks around. You get winded climbing stairs, even if you used to be fine. This goes on for weeks or months. People often think they’re just getting out of shape-or have a lingering cold. Then there’s chronic HP. This is the dangerous one. You’ve been exposed to the trigger for months or years. Your lungs start to scar. The cough doesn’t go away. You lose weight without trying. Your fingers might even club-curving at the tips. At this stage, the damage can be permanent. Pulmonary fibrosis sets in. Your lungs stiffen. Breathing becomes a constant effort.What Triggers It (And What Doesn’t)
Here’s where people get confused. Medications like amiodarone, nitrofurantoin, or chemotherapy drugs can cause lung inflammation. But that’s not hypersensitivity pneumonitis. That’s drug-induced lung injury. The immune response is different. The pattern of scarring is different. And crucially, you don’t need to inhale those drugs-they’re taken by mouth or IV. True HP comes from things you breathe in:- Bird proteins-from feathers, droppings, or dust around parrots, pigeons, chickens, or even pet birds. This is called bird fancier’s lung.
- Moldy hay or grain-farmers, barn workers, and people who handle stored grain get farmer’s lung.
- Fungi in humidifiers or air conditioners-especially if the water isn’t changed regularly. The bacteria in the water get aerosolized and inhaled.
- Mushroom spores-workers in mushroom farms are at risk.
- Hot tub biofilm-mold and bacteria in the warm, wet environment can become airborne when the tub is used.
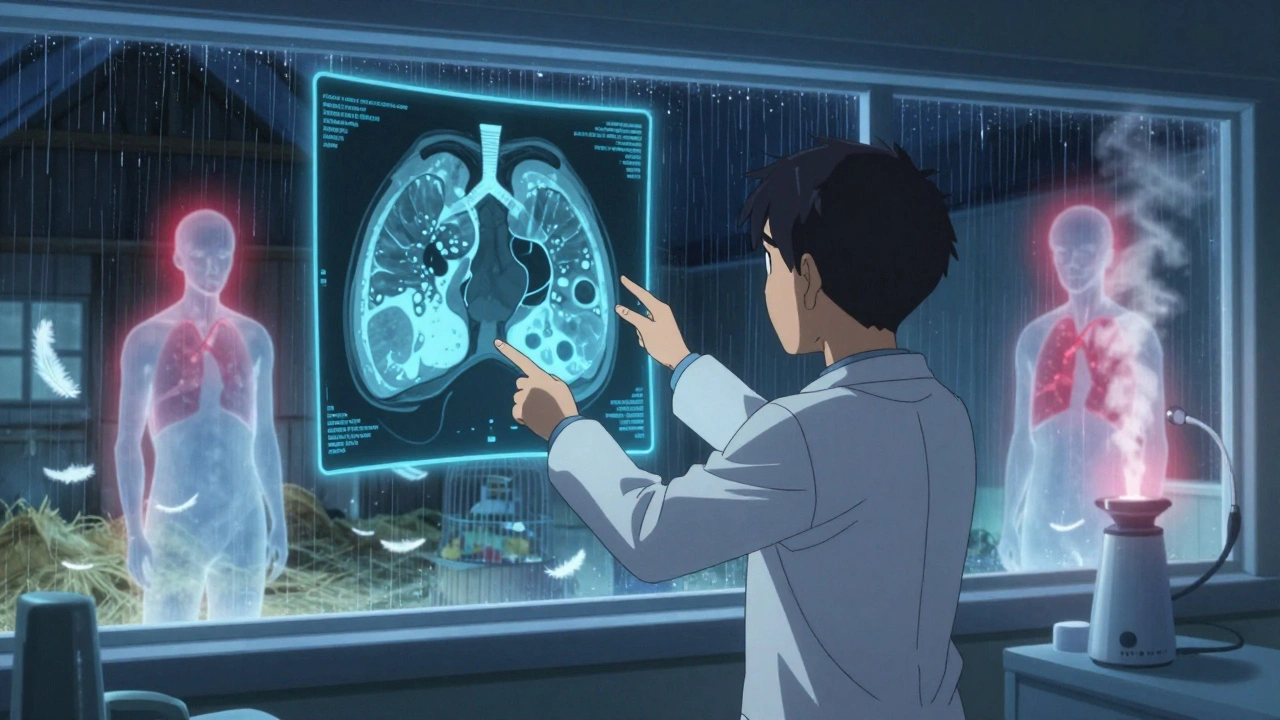
How Doctors Diagnose It
There’s no single blood test for HP. Diagnosis is like solving a puzzle. Doctors look at five things:- Your history-Do your symptoms get worse at work? After cleaning the birdcage? After using the humidifier? Do they improve when you’re away from home or work?
- Imaging-A high-resolution CT scan of your chest shows telltale signs: patchy ground-glass shadows, mosaic patterns, and air trapping (especially on exhale scans).
- Blood tests-They check for antibodies to specific antigens. If you’ve been around birds, they’ll test for pigeon serum proteins. If you’re a farmer, they’ll test for mold from hay. These antibodies are found in 60-90% of cases.
- Bronchoalveolar lavage-A small tube is passed into your lungs, and fluid is washed out. If more than 40% of the cells are lymphocytes (a type of white blood cell), it’s a strong clue for HP.
- Lung biopsy-In unclear cases, a small sample of lung tissue shows poorly formed granulomas and lymphocyte buildup around the small airways. That’s the fingerprint of HP.
Treatment: Stop the Exposure
The most important treatment isn’t a drug. It’s avoidance. If you catch HP early-in the acute or subacute stage-and you stop breathing in the trigger, your lungs can heal completely. Studies show 70-80% of people recover fully with just removal of the antigen. For more severe cases, doctors may prescribe short-term steroids like prednisone to calm the inflammation. But steroids won’t fix the problem if you keep breathing in the dust. You’ll just be masking it-and risking permanent damage. In chronic HP, where scarring has already started, treatment gets harder. Steroids may help slow inflammation, but antifibrotic drugs like nintedanib (used in idiopathic pulmonary fibrosis) are now being tested in HP. One trial showed a 56% reduction in lung function decline over a year. Pulmonary rehab-breathing exercises, walking programs, oxygen therapy-helps manage symptoms. If your oxygen levels drop below 88%, you’ll need supplemental oxygen at home.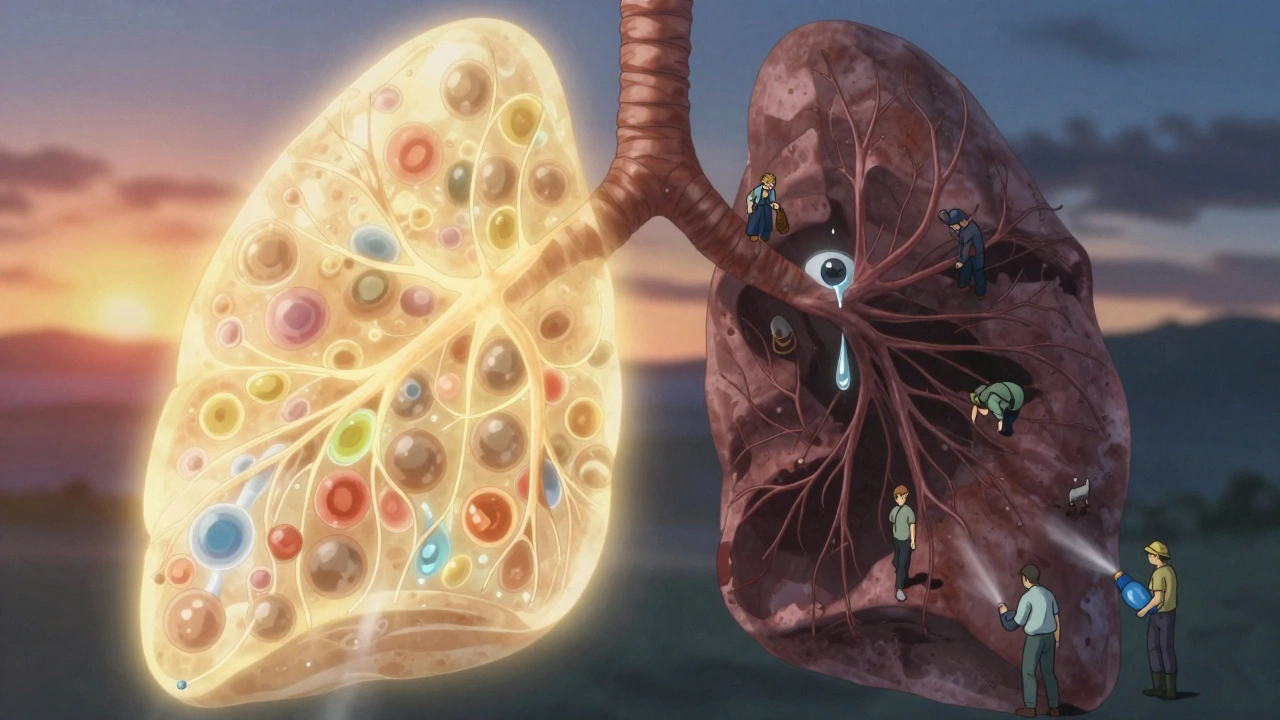
What Happens If You Don’t Act
Ignoring HP is dangerous. The longer you’re exposed, the more your lungs scar. Once fibrosis sets in, it’s irreversible. The 5-year survival rate for chronic HP ranges from 50% to 80%, depending on how much scarring is already there. If you’re a bird owner and your cough won’t go away, don’t assume it’s just dust. If you work in agriculture and get winded faster than your coworkers, don’t brush it off as aging. If you use a humidifier and feel worse every morning, clean it-or stop using it. Cigarette smoking, oddly enough, seems to lower your risk of developing HP. That’s not a recommendation-it’s just a curious observation from studies. Smoking damages your lungs in other ways, so don’t use this as an excuse to smoke.When to See a Doctor
See a pulmonologist if:- Your cough lasts more than 2 weeks without a clear cause
- You get short of breath doing things you used to handle easily
- Your symptoms improve when you’re away from home or work
- You own birds, work with grain, or use a humidifier regularly
Final Thought: It’s Not Your Pill-It’s Your Air
We live in a world where every symptom gets blamed on a medication. But sometimes, the culprit isn’t in your medicine cabinet. It’s in your garage, your basement, your birdcage, or your humidifier. Hypersensitivity pneumonitis teaches us that lungs don’t just react to what you swallow. They react to what you breathe. And if you’re coughing and short of breath, it’s worth asking: what’s in the air around you?Can medications cause hypersensitivity pneumonitis?
No, medications do not cause true hypersensitivity pneumonitis. While some drugs like amiodarone or nitrofurantoin can cause lung inflammation, this is classified as drug-induced interstitial lung disease (DILD), not HP. HP requires inhalation of airborne antigens like bird proteins or mold. The immune response, location of damage, and lung tissue patterns are different. Medications are swallowed or injected-they don’t trigger the specific alveolar inflammation seen in HP.
What’s the difference between hypersensitivity pneumonitis and asthma?
Asthma affects the airways (bronchi), causing wheezing, chest tightness, and reversible airflow blockage. Hypersensitivity pneumonitis affects the lung tissue itself-the alveoli-and causes inflammation, scarring, and reduced oxygen transfer. Asthma responds to inhalers; HP does not. HP symptoms improve when you leave the trigger environment, while asthma often flares with exercise or allergens like pollen.
Is hypersensitivity pneumonitis rare?
It’s uncommon in the general population-about 1 to 2 cases per 100,000 people each year. But in high-risk groups, it’s much more common. Farmers, bird owners, and workers in mushroom farms or humidifier maintenance can have rates up to 10 times higher. Many cases go undiagnosed because symptoms are mistaken for bronchitis or aging.
Can I get HP from my home humidifier?
Yes. If your humidifier isn’t cleaned regularly, bacteria and mold can grow in the water tank. When the device runs, it sprays these particles into the air. Inhaling them over time can trigger hypersensitivity pneumonitis, sometimes called ‘humidifier lung.’ People who use humidifiers daily, especially in winter, are at risk. Cleaning the tank weekly with vinegar or bleach and using distilled water reduces the risk significantly.
How long does it take to recover from hypersensitivity pneumonitis?
Recovery depends on the stage. In acute HP, symptoms often disappear within 24 to 48 hours after avoiding the trigger. Subacute cases may take weeks to months to improve. Chronic HP with scarring may never fully reverse, though stopping exposure can prevent further damage. Early action is critical-the sooner you remove the trigger, the better your chance of full recovery.


9 Comments
December 2, 2025 Arun kumar
man i had this weird cough for months and thought it was just allergies till i cleaned my humidifier and poof-gone. never thought it was something like this. thanks for laying it out like this.
December 2, 2025 Ella van Rij
oh so THAT’S why my ‘bird fancier’s lung’ diagnosis got me side-eyed at the clinic last year. everyone assumed i was just some weirdo with too many parrots. turns out i’m just a victim of airborne pigeon drama. 🙃
December 3, 2025 Zed theMartian
of course the only people who get this are the ones who can afford bird cages, humidifiers, and fancy CT scans. Meanwhile, the working class is coughing up lung tissue from factory dust and being told to ‘take a puff of albuterol.’ this is elite medicine for elite problems. 🤡
December 3, 2025 Steve World Shopping
the immunopathological cascade triggered by inhaled particulate antigens is a well-documented phenomenon in occupational pulmonology, particularly in the context of type III hypersensitivity reactions. the alveolar lymphocytic infiltration pattern is diagnostic when correlated with exposure history. many clinicians miss this due to cognitive bias toward pharmaceutical etiologies.
December 5, 2025 Rebecca M.
so let me get this straight… if i stop using my humidifier, i don’t need to take meds? but if i use a $300 diffuser with ‘essential oils’ it’s totally fine? please. i’m not buying it. this is just a fancy way of saying ‘stop being lazy and clean your shit.’
December 6, 2025 ATUL BHARDWAJ
in India many farmers ignore this till they can’t walk. we call it ‘dust lung’ but no doctor listens. your post is right. simple things kill quietly.
December 7, 2025 Jack Dao
you people are ridiculous. you blame humidifiers and birds like they’re the enemy. the real issue is that modern life has made us so fragile we can’t handle a little dust. back in my day, we breathed mold, bird crap, and diesel fumes and still ran marathons. now everyone’s wheezing because their cat sneezed near the air purifier.
also, ‘pulmonary rehab’? that’s just a fancy gym for people who can’t breathe. get off the couch and walk. your lungs aren’t made of porcelain.
and don’t get me started on steroids. you think prednisone fixes anything? it just hides the problem until your body collapses from the side effects. the only cure is discipline. stop being a baby.
also, if you’re using distilled water in your humidifier, you’re wasting money. tap water is fine. the bacteria are harmless unless you’re already immunocompromised. which, statistically, you probably are because you read medical blogs instead of going outside.
and yes, smoking reduces risk. not because it’s good, but because it kills off the immune cells that overreact. ironic, isn’t it? the thing that destroys your lungs also prevents this specific form of destruction. the universe has a sick sense of humor.
you want to live longer? stop obsessing over every breath. breathe. get dirty. live. stop treating your lungs like a museum exhibit.
and no, you can’t ‘test for antibodies’ and call it diagnosis. that’s pseudoscience with a lab coat. real medicine is observation. if your cough goes away when you leave home? then your home is the problem. fix it. don’t pay a specialist $500 to tell you what you already know.
December 7, 2025 Lynn Steiner
i cried reading this. i lost my dad to this. he was a pigeon fancier. he ignored it for years because ‘everyone gets a cough in winter.’ he was 62. they told him it was COPD. it wasn’t. it was his birds. he never knew. i wish i’d known sooner. now i clean my humidifier every 3 days. no excuses.
December 8, 2025 Alicia Marks
you’re not alone. if you’re reading this and have a cough that won’t quit-don’t wait. check your humidifier. clean your birdcage. breathe easy. you’ve got this.
Write a comment