When you pick up a generic pill at the pharmacy, you might wonder: is this really the same as the brand-name version? The answer isn’t just yes-it’s backed by one of the most rigorous drug approval systems in the world. The FDA doesn’t just approve generic drugs because they’re cheaper. They approve them because they must meet the same quality, strength, purity, and stability standards as the original brand-name drug. This isn’t guesswork. It’s science, enforced by law and tested in labs across the globe.
What Makes a Generic Drug Legally Equivalent?
The legal foundation for generic drugs in the U.S. comes from the Hatch-Waxman Act of 1984. This law created a clear path for generic manufacturers to bring affordable versions of drugs to market without repeating every expensive clinical trial the original maker did. But here’s the catch: they still have to prove their product works the same way.
Two key terms define this equivalence: pharmaceutical equivalence and bioequivalence.
Pharmaceutical equivalence means the generic drug has the exact same active ingredient, strength, dosage form (tablet, capsule, injection), and route of administration (oral, intravenous, etc.) as the brand-name drug. The label must also list the same uses and warnings. That’s non-negotiable.
But what about the color? The shape? The filler ingredients? Those can be different. A generic metformin tablet might be white and oval instead of blue and round. It might use a different starch or dye. Those are inactive ingredients-called excipients-and the FDA allows minor differences as long as they don’t affect how the drug works in your body.
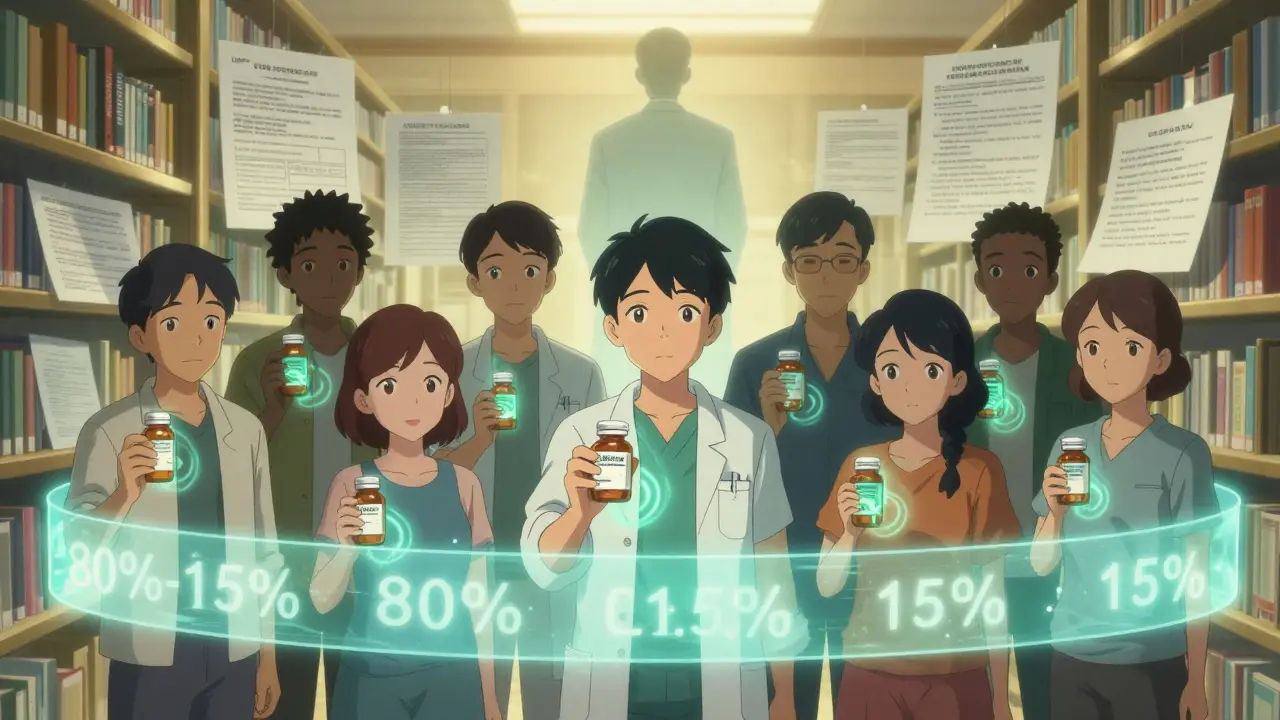
Bioequivalence is where the real testing happens. It’s not enough for a generic to have the same ingredient. It has to release that ingredient into your bloodstream at the same rate and to the same extent as the brand-name drug. That’s measured through blood tests in healthy volunteers. For most small-molecule generics, the FDA requires a study with 24 to 36 people who take both the generic and brand versions under controlled conditions. Then scientists compare two key numbers: Cmax (how high the drug peaks in your blood) and AUC (how much of the drug gets absorbed over time).
The FDA’s rule? The 90% confidence interval for both values must fall between 80% and 125%. That’s not a wide range-it’s tight. It means the generic’s absorption can’t be more than 20% lower or 25% higher than the brand. If it’s outside that range, the application gets rejected. No exceptions.
How the FDA Ensures Manufacturing Quality
Even if a drug works the same in a lab, it can still be dangerous if it’s made in a dirty or sloppy facility. That’s why the FDA enforces Current Good Manufacturing Practices (cGMP), written into federal law under 21 CFR Parts 210 and 211. These rules apply equally to brand-name and generic manufacturers-no special treatment for either.
cGMP covers everything: how raw materials are received and stored, how equipment is cleaned and calibrated, how workers are trained, how batches are tested before release. Every step has to be documented. Every test method has to be validated. There’s no room for shortcuts.
The FDA doesn’t trust paperwork alone. They send inspectors-over 3,500 inspections a year-to factories around the world. These aren’t surprise visits. They’re planned, detailed, and often last weeks. Inspectors check logs, review data, walk through clean rooms, and even test samples on the spot. If they find a pattern of violations, the facility can be shut down. The FDA doesn’t just say, “Fix it.” They say, “Stop shipping.”
Here’s something many people don’t know: about half of all generic drugs sold in the U.S. are made by the same companies that produce the original brand-name versions. In many cases, they’re made on the same production lines. That’s not a loophole-it’s a feature. It means the same quality controls, the same engineers, the same audits. If you’re buying a generic made by Pfizer or Merck, you’re getting the same facility that made the brand-name version.

The ANDA Process: How a Generic Gets Approved
Generic manufacturers don’t file a full New Drug Application (NDA) like brand-name companies do. Instead, they submit an Abbreviated New Drug Application, or ANDA. The word “abbreviated” is misleading-it’s still a massive, complex document. It includes detailed chemistry data, manufacturing protocols, stability studies, and bioequivalence results.
The FDA’s Office of Generic Drugs (OGD) reviews each ANDA. They have 10 months to complete a standard review under the Generic Drug User Fee Amendments (GDUFA), which was first introduced in 2012 and renewed in 2022. GDUFA gave the FDA more funding and staff to speed things up. Today, the OGD has 750 employees dedicated solely to reviewing generics.
Stability testing is one of the most time-consuming parts. Manufacturers must prove their product won’t break down over time. They store samples at high heat and humidity (40°C/75% RH) for six months and keep them at normal storage conditions for 12 to 24 months. If the drug degrades too fast, or if impurities form, the FDA won’t approve it.
Batch testing is another requirement. Every single batch of a generic drug must be tested for identity, strength, purity, and dissolution. These aren’t spot checks-they’re mandatory for every lot. The FDA also requires manufacturers to follow compendial standards like those in the United States Pharmacopeia (USP), or submit their own validated methods if the drug is too complex.
Between 2022 and 2023, the FDA approved 892 original ANDAs and issued 478 complete response letters-meaning the application was rejected due to missing or flawed data. That’s a rejection rate of over 35%. Approval isn’t guaranteed. It’s earned.
Complex Generics: When Simple Tests Aren’t Enough
Not all drugs are as straightforward as a tablet you swallow. Some-like inhalers, topical creams, injectables, or eye drops-are harder to copy. These are called complex generics. For these, measuring blood levels isn’t enough. The drug’s physical structure matters.
Take an asthma inhaler. The brand-name version delivers a fine mist of medication in a specific particle size. A generic version might have the same chemical, but if the propellant or nozzle design is off, the particles won’t reach the lungs the same way. That’s why the FDA developed over 2,143 product-specific guidances as of 2023. These are detailed scientific blueprints for how to prove equivalence for each complex product.
For some of these, the FDA now requires additional testing: in vitro dissolution profiles, particle size analysis, or even clinical endpoint studies where patients are monitored for actual health outcomes-not just blood levels. In 2022, the FDA identified that 17% of complex generic categories needed these extra steps. The agency has invested $15.7 million in research to develop better testing methods, and they host public workshops to bring scientists, manufacturers, and regulators together.
Dr. Charles Ganley, former head of the FDA’s Office of Generic Drugs, pointed out in 2019 that these products are “the new frontier” for generic approval. “You can’t just measure blood concentration,” he said. “You have to measure how the drug behaves in the body, not just how much gets in.”
Are Generic Drugs Safe? Real-World Data
Over 90% of prescriptions filled in the U.S. are for generic drugs. That’s more than 4 billion prescriptions a year. And yet, some people still worry.
Consumer Reports surveyed 1,200 U.S. adults in 2022. Eighty-nine percent said they were satisfied with their generic medications. Sixty-two percent said they chose generics specifically to save money. That’s trust built on experience.
But there are exceptions. For drugs with a narrow therapeutic index-where even a small change in blood level can cause harm-some patients report issues. Levothyroxine, used for thyroid conditions, is one. A 2021 study in JAMA Internal Medicine found that 12.3% of patients switching between different generic versions experienced thyroid hormone fluctuations that required dose adjustments. That’s why doctors often recommend staying on the same generic brand for these drugs.
On Reddit’s r/pharmacy community, a 2023 thread with over 1,400 responses showed 83% of users reported no difference between generic and brand-name drugs. The remaining 17% mostly cited problems with seizure medications or blood thinners like warfarin. These are rare cases, but they matter. That’s why the FDA continues to monitor adverse event reports and encourages prescribers to report any issues.
The American Medical Association, the American Academy of Family Physicians, and the FDA all agree: FDA-approved generics are safe and effective. The data backs it up. Generic drugs saved the U.S. healthcare system $37 billion in 2022 alone. They make up only 23% of total drug spending, even though they’re used in over 90% of prescriptions.
What This Means for You
If you’re prescribed a generic drug, you’re not getting a second-rate product. You’re getting a drug that passed the same tests, met the same standards, and was made under the same rules as the brand-name version. The FDA doesn’t lower the bar for generics-they make sure every pill, capsule, or injection you take is safe, effective, and consistent.
There are rare cases where switching generics might cause issues, especially with narrow therapeutic index drugs. If you notice a change in how you feel after switching, talk to your doctor. But don’t assume the generic is to blame. Most of the time, it’s not.
The system works because it’s transparent, science-based, and relentlessly enforced. Generic drugs aren’t cheaper because they’re worse. They’re cheaper because the system is designed to cut out unnecessary costs-not quality.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence-meaning they deliver the same amount of drug into your bloodstream at the same rate. Over 90% of prescriptions in the U.S. are for generics, and studies consistently show they work just as well.
Why do generic drugs look different from brand-name drugs?
The law allows differences in color, shape, size, and inactive ingredients like dyes or fillers. These don’t affect how the drug works. The active ingredient must be identical. The differences are mostly for trademark reasons-brand-name companies can’t copyright the drug itself, but they can trademark its appearance.
Does the FDA inspect generic drug factories?
Yes. The FDA conducts over 3,500 inspections each year at manufacturing sites worldwide, including those making generics. These inspections check compliance with Current Good Manufacturing Practices (cGMP). Many generic drugs are made in the same facilities as brand-name drugs-even by the same companies.
Are all generic drugs approved the same way?
No. Most small-molecule generics are approved based on bioequivalence studies in healthy volunteers. But complex products like inhalers, topical creams, or long-acting injectables require additional testing-such as particle size analysis, in vitro dissolution, or clinical endpoint studies-because blood levels alone can’t prove equivalence.
Can switching between different generic brands cause problems?
For most drugs, no. But for medications with a narrow therapeutic index-like levothyroxine, warfarin, or some seizure drugs-even small changes in absorption can matter. Some patients report side effects after switching between different generic versions. If you notice a change in how you feel, talk to your doctor. You may need to stick with one brand of generic.
How long does it take for a generic drug to be approved?
Under the Generic Drug User Fee Amendments (GDUFA), the FDA aims to complete a standard review of an Abbreviated New Drug Application (ANDA) in 10 months. Complex applications or those with missing data may take longer. In 2022, the FDA approved 892 original ANDAs and issued 478 complete response letters, showing the process is rigorous and selective.


13 Comments
December 16, 2025 Jonathan Morris
The FDA doesn't inspect every single batch. They sample. And those labs? Half are in India and China. The cGMP reports are self-submitted. You think they're checking every vial? Please. This is corporate theater with a science veneer. I've seen the whistleblower reports. The data gets cooked. The inspectors get dinner paid for. It's not regulation-it's a sponsorship deal.
December 17, 2025 Donna Packard
I’ve been on generic levothyroxine for years and never had an issue. My doctor switched me to save money, and I feel just fine. It’s nice to know the system’s actually working for people like us who can’t afford brand names.
December 19, 2025 Patrick A. Ck. Trip
While I appreciate the thoroughness of the FDA's oversight framework, I must express a note of cautious optimism regarding the global supply chain's integrity. The statistical probability of contamination or deviation increases exponentially with the number of manufacturing sites, particularly in jurisdictions with less stringent regulatory enforcement. That said, the 80-125% bioequivalence window remains scientifically defensible.
December 21, 2025 Virginia Seitz
Generics saved my life 💙 no joke. I take 5 meds and all are generic. My wallet and my body thank you 🙏
December 22, 2025 Peter Ronai
Oh wow, the FDA is a saint? Tell that to the 17% of complex generics that got approved with flawed dissolution profiles. And don’t get me started on the 35% rejection rate-those are the ones that passed the first round. The rest? Buried. The system is a rigged casino and you’re all just betting on the house.
December 23, 2025 Steven Lavoie
I’ve worked in a compounding pharmacy for 12 years. I’ve seen generics from the same manufacturer that look identical to brand-name pills-same size, same color, same imprint. The only difference is the label. And yes, the lab tests confirm equivalence. People are scared of what they don’t understand. But the science is solid.
December 24, 2025 Jane Wei
My cousin switched from brand to generic Adderall and had a full-blown panic attack. Turned out it was the filler-she’s allergic to the dye. Not the drug. Just the color. So yeah, sometimes it matters. But 9 times outta 10? Totally fine.
December 24, 2025 Jody Patrick
Why are we letting foreign factories make our medicine? We used to make this stuff here. Now we’re trusting some guy in Bangalore with our lives. This isn’t freedom. It’s surrender.
December 25, 2025 Radhika M
My uncle in India takes generic insulin. He pays $2 a vial. In US, same vial costs $100. FDA rules are same. So why the price difference? Because of how the system works here. Not because the drug is different.
December 27, 2025 Philippa Skiadopoulou
The bioequivalence standards are robust. The challenge lies in enforcement consistency across jurisdictions. Regulatory harmonization remains an aspiration rather than a reality. That said, the data supporting generic efficacy remains compelling.
December 29, 2025 Pawan Chaudhary
My mom uses generic blood pressure pills. She says she feels better now because she can afford to take them every day. That’s what matters. Science is great, but real life is about access. Thanks for making it possible.
December 29, 2025 Linda Caldwell
Generics aren’t cheap because they’re bad-they’re cheap because the system stopped letting pharma companies charge $500 for a pill that costs $2 to make. This is capitalism working the way it should. No magic, no conspiracy. Just smart policy.
December 30, 2025 Anna Giakoumakatou
How delightful. A 200-page pamphlet on how the FDA pretends to regulate. Tell me again how this isn’t just a PR campaign designed to make the public feel safe while corporations siphon billions from Medicaid? I mean, the very fact that you need a 10-month review for a pill that’s been around since 1998… it’s almost poetic.
Write a comment