When you pick up a new prescription, the small booklet that comes with it isn’t just filler. It’s your first line of defense against accidental overdose. Most people glance at the dosing instructions and toss it aside. But buried in those pages are critical details about what happens if you take too much - and what to do next. If you or someone you care about is on medications like opioids, benzodiazepines, or even certain antidepressants, knowing how to read those warnings could save a life.
Start with the Boxed Warning
Look for a black border around a section at the top of the guide. That’s the Boxed Warning - the strongest alert the FDA requires. It’s not there for decoration. If your medication has one, it means there’s a serious risk of overdose, respiratory depression, or death, especially when mixed with other drugs. For example, opioid painkillers like oxycodone or hydrocodone often carry a Boxed Warning about respiratory failure. Benzodiazepines like diazepam or alprazolam warn about fatal interactions with alcohol or opioids. Don’t skip this part. It’s the clearest signal that you need to be extra careful.
Find the Overdosage Section
Scroll down until you see a heading that says Overdosage. This section is required by law to be included in every prescription medication guide in the U.S. and the UK. It doesn’t give you a magic number like “30 pills = overdose.” Instead, it tells you what happens when too much is taken. For example, it might say: “Ingestion of more than 100 mg of tramadol may cause seizures, altered mental status, and respiratory depression.” Or: “Acute ingestion of 200 mg or more of fluoxetine has been associated with serotonin syndrome.” These aren’t guesses - they’re based on clinical reports and poison control data.
Pay attention to symptoms listed here. They’re not vague. They’re specific: “slowed breathing,” “unresponsiveness,” “blue lips,” “seizures,” “rigid muscles.” These are the same signs emergency responders look for. If you recognize them in yourself or someone else, don’t wait. Act immediately.
Locate the Antidote Information
Right after the Overdosage section, look for the word Antidote or Treatment. This is where you’ll find what can reverse or reduce the effects of an overdose. For opioids, it’s almost always naloxone. The guide will tell you it’s available as a nasal spray or injection and may note that multiple doses may be needed. For benzodiazepine overdoses, it might mention flumazenil - though this is rarely used outside hospitals due to risks. For serotonin syndrome caused by SSRIs, it might say cyproheptadine or supportive care.
Don’t assume you’ll know what to do if you don’t read this. Naloxone isn’t listed in the dosing section - it’s only in the overdose part. If you’re on an opioid, ask your pharmacist for a prescription for naloxone. Many pharmacies now offer it without a prescription. Keep it where you keep your medication. Know how to use it. Practice with a training device.

Check the Warnings and Precautions
This section is longer and more detailed. It’s where you’ll find hidden dangers. For example, it might say: “Avoid alcohol. May increase risk of central nervous system depression.” Or: “Use with caution in patients with liver impairment - reduced clearance may lead to accumulation.” These aren’t just general cautions. They’re red flags for overdose risk. If you have liver disease, kidney problems, or are over 65, your body processes drugs slower. That means the same dose that’s safe for someone else could become toxic for you.
Also look for mentions of drug interactions. If your guide says “Concomitant use with CYP3A4 inhibitors may increase plasma concentrations,” that’s medical jargon for: “Don’t take this with grapefruit juice, certain antibiotics, or antifungals - it can build up to dangerous levels.” Even over-the-counter meds like ibuprofen or cold remedies can interact. Write down all your medications - including supplements - and bring them to every appointment.
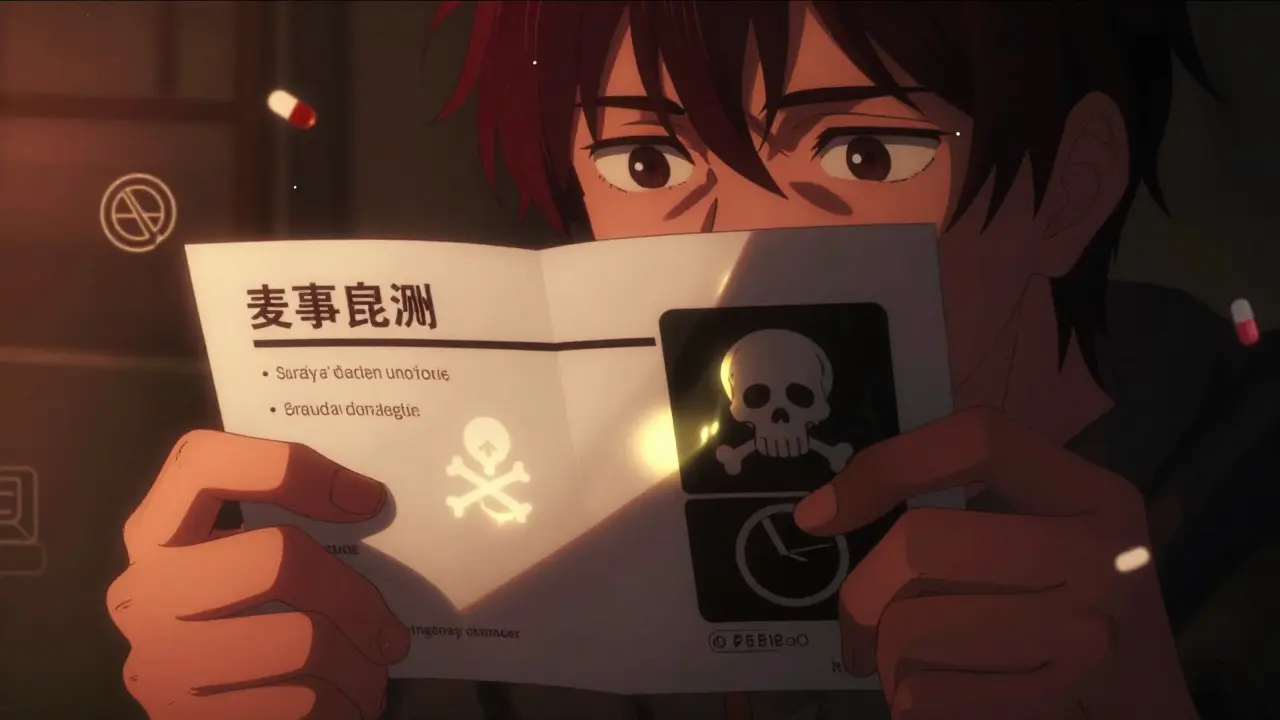
Understand the Symbols and Icons
Many newer medication guides use icons to highlight risks. A skull and crossbones means severe toxicity risk. A circle with a slash through it means “do not combine.” A downward arrow might mean “risk increases with higher doses.” These aren’t universal, but they’re becoming more common. If you see one you don’t recognize, ask your pharmacist. Don’t guess. A single misread symbol can lead to a fatal mistake.

Know What’s Missing
Medication guides don’t cover everything. They won’t tell you how long it takes for an overdose to become fatal. They won’t say if your risk goes up after a few days of use. They won’t warn you about tolerance changes after a hospital stay. That’s why you need to pair this guide with real-world knowledge. If you’ve been on a medication for months and suddenly feel dizzy or unusually sleepy, don’t assume it’s just stress. Check the guide again. Your body may be reacting differently.
Also, guides are written for the average adult. They don’t adjust for weight, age, or metabolism. If you’re under 120 pounds or over 75, you’re at higher risk - even if you’re taking the “recommended” dose. Talk to your doctor about whether your dose is right for you.
Keep It Accessible
Don’t tuck the guide away in a drawer. Tape it to the inside of your medicine cabinet. Keep a digital copy on your phone. Share it with a family member or roommate. Make sure someone else knows where to find it - and what to do if you can’t speak for yourself. Many overdoses happen when people are alone. If your guide says naloxone is the antidote, make sure your partner or neighbor knows where it is and how to use it. Practice with them. Turn it into a routine, like checking your smoke detector.
When in Doubt, Call Poison Control
Every medication guide lists a poison control number - usually at the bottom of the first page. In the U.S., it’s 1-800-222-1222. In the UK, it’s 111 or your local emergency number. Don’t wait for symptoms to worsen. If you think you’ve taken too much - even if you’re not sure - call immediately. Poison control experts have access to real-time databases on drug toxicity and can guide you through what to do next. They’ve seen it all. They won’t judge. They’ll help.
Reading a medication guide isn’t about being paranoid. It’s about being prepared. You wouldn’t drive a car without checking the brakes. Don’t take a powerful medication without knowing what happens if something goes wrong. The guide is your roadmap. Use it.

8 Comments
December 15, 2025 Harriet Wollaston
I never realized how much life-saving info is buried in those little booklets. I used to toss mine right after checking the dose. Now I keep mine taped to my medicine cabinet next to my naloxone. My mom’s on opioids, and I made sure she knows how to use it too. It’s weird to think a tiny pamphlet could be the difference between life and death, but it really is.
December 15, 2025 Lauren Scrima
Wow. A box. With a border. And words. Who knew?? 😏
December 17, 2025 sharon soila
Reading this guide is not just a smart choice-it is a moral responsibility. Every person who takes medication has a duty to understand its power, its danger, and its rescue. This is not fear. This is care. This is love in action. Keep the guide. Share the knowledge. Save a life today.
December 17, 2025 nina nakamura
People still need a guide for this? You’re telling me you don’t already know not to mix benzos with alcohol? You’re telling me you don’t know opioids can stop your breathing? This isn’t rocket science. If you can’t read a 10-page pamphlet without getting overwhelmed, maybe you shouldn’t be taking controlled substances at all.
December 18, 2025 Alvin Montanez
Let me tell you something. I’ve been in the medical field for 22 years. I’ve seen people die because they didn’t read the damn guide. I’ve seen grandmas take extra pills because they thought ‘it’s just a little more’ and then they couldn’t wake up. I’ve seen husbands forget their wives are on SSRIs and give them cold medicine with dextromethorphan and then they end up in the ICU with serotonin syndrome. This isn’t theoretical. This is real. And if you’re not reading the guide, you’re gambling with someone’s life. And that’s not just irresponsible-it’s selfish.
December 18, 2025 Lara Tobin
This made me cry 😭 I showed my brother the naloxone part and he actually got a prescription today. He’s been on oxycodone for years and never knew. I’m so glad someone wrote this. Thank you.
December 19, 2025 Jamie Clark
These guides are a band-aid on a bullet wound. The real problem is that pharmaceutical companies are allowed to pump out deadly drugs with zero accountability. They bury the risks in fine print while marketing them like candy. Naloxone should be as common as aspirin. It should be in every vending machine, every gas station, every public bathroom. We’re treating overdose like a personal failure instead of a public health emergency. This guide? It’s a survival manual for a system that refuses to fix itself.
December 19, 2025 Keasha Trawick
Okay, so imagine your meds are a dragon. The Boxed Warning? That’s the dragon’s glowing eyes and smoke curling from its nostrils. The Overdosage section? That’s the dragon’s breath-hot, toxic, and lethal. The Antidote? That’s the magic sword-naloxone, flumazenil, cyproheptadine-shiny, rare, and only works if you know where to stab. And the symbols? Those are runes carved by ancient pharmacists to warn the uninitiated. Skip the guide? You’re walking into the cave without a torch, a sword, or a prayer. Don’t be the hero who dies because they didn’t read the scroll.
Write a comment