When your skin breaks out in thick, red, scaly patches, it’s easy to think it’s just a cosmetic problem. But if those patches come with stiff, swollen fingers, aching heels, or lower back pain, you’re not just dealing with a skin condition-you’re facing something deeper. Psoriatic arthritis is what happens when the same immune system mistake that causes psoriasis starts attacking your joints. It’s not two separate diseases. It’s one autoimmune condition showing up in two places at once.
How Psoriasis Turns Into Psoriatic Arthritis
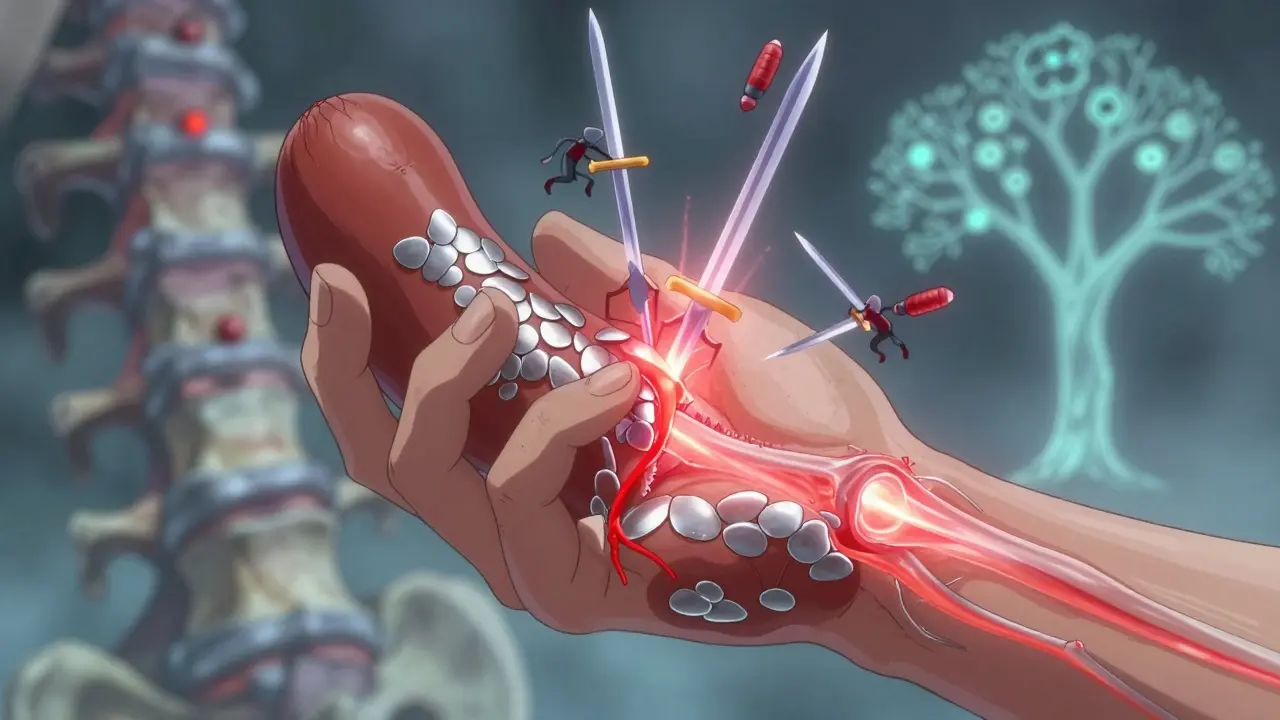
About 30% of people with psoriasis will develop psoriatic arthritis. For most, the skin comes first-often years before the joints start acting up. In 85% of cases, psoriasis shows up before any joint pain. But in 5 to 10% of cases, the joints hurt first, and the skin rash follows later. That’s why doctors don’t always catch it right away. The immune system in people with psoriatic arthritis gets confused. It starts attacking healthy skin cells and joint tissues as if they’re invaders. This triggers inflammation-not just on the surface, but deep inside the joints, tendons, and even where ligaments attach to bone. The result? Pain, swelling, and over time, permanent damage. It’s not random who gets it. Genetics play a big role. If you have a close relative with psoriasis or arthritis, your risk goes up. Specific genes like HLA-B27, HLA-B38, and HLA-B39 are linked to higher chances of developing psoriatic arthritis. But genes alone don’t decide it. Stress, infections, obesity, and even gut bacteria can push the immune system over the edge.The Signs You Can’t Ignore
Psoriatic arthritis doesn’t just affect one joint. It hits multiple areas in different ways. Here’s what to watch for:- Dactylitis-your fingers or toes swell up like sausages. This happens in about 40% of people with PsA and is a major red flag.
- Enthesitis-pain where tendons or ligaments meet bone. Think Achilles tendon pain or soreness under the foot. It affects 35 to 50% of patients.
- Nail changes-pitting, ridges, or nails lifting off the nail bed. Up to 80% of people with PsA have these changes.
- Spinal stiffness-lower back or neck pain that’s worse in the morning and improves with movement. This signals axial involvement, which can lead to fused vertebrae if untreated.
- Joint swelling-knees, wrists, ankles, even small joints in the hands and feet. The swelling is often uneven-some joints affected, others untouched.
And yes, the skin plaques are still there. Red, raised patches covered in silvery scales, usually on elbows, knees, scalp, or lower back. But here’s the catch: the severity of your skin rash doesn’t match the severity of your joint damage. Someone with mild psoriasis can have severe arthritis-and vice versa.
How Doctors Diagnose It
There’s no single blood test for psoriatic arthritis. Diagnosis is a puzzle. Doctors use the CASPAR criteria, a set of rules developed in 2006 that’s now the gold standard. To be diagnosed, you need inflammatory joint disease plus at least three points from these clues:- Current psoriasis (3 points)
- History of psoriasis (2 points)
- Nail changes (1 point)
- Negative rheumatoid factor (1 point)
- Typical bone changes on X-ray (1 point)
A score of 3 or higher means PsA. That’s 91% accurate at spotting it and 99% good at ruling it out.
Doctors also check:
- Blood tests for inflammation markers like CRP and ESR
- Imaging-X-rays show bone erosion or the unique "pencil-in-cup" deformity in 30-40% of cases
- Ultrasound or MRI to catch early inflammation before it shows on X-rays
- Skin biopsy, if there’s doubt about whether it’s psoriasis or another condition like eczema
Family history matters too. If your mom or brother has psoriasis, that’s a big clue.
What Happens If You Don’t Treat It
Left unchecked, psoriatic arthritis doesn’t just hurt-it breaks you down. About 60-70% of people with established PsA show bone erosion on imaging. Over time, joints can become deformed, stiff, and useless. Finger joints might fuse. Spinal segments can lock together. Mobility drops. Quality of life plummets. But the damage isn’t just in the joints. PsA is a full-body disease. People with PsA have a 43% higher risk of heart attack than the general population. Nearly half have metabolic syndrome-high blood pressure, belly fat, insulin resistance, and bad cholesterol. Depression and anxiety are twice as common. Studies show quality of life scores are 30-40% lower than in people without PsA. And here’s the scary part: mortality is 30-50% higher in PsA patients. Not because of the arthritis itself-but because of the heart disease, stroke, and diabetes that come with it.Treatment That Actually Works
The goal isn’t just to reduce pain. It’s to stop the immune system from destroying your body. The new standard is called minimal disease activity-a set of strict targets:- Tender joints: 1 or fewer
- Swollen joints: 1 or fewer
- Skin involvement: 1% or less of body surface
- Pain score: 15mm or less on a 100mm scale
- Global health score: 20mm or less
- Physical function (HAQ): 0.5 or lower
- No fatigue
Getting there takes a step-by-step approach.
Step 1: NSAIDs-like ibuprofen or naproxen. They help with pain and swelling, but they don’t stop joint damage.
Step 2: Traditional DMARDs-methotrexate is the go-to. It slows the immune system’s attack. Works for about half of people, especially if joint swelling is the main problem.
Step 3: Biologics-these are the game-changers. They target specific parts of the immune system:
- TNF inhibitors (adalimumab, etanercept, infliximab): Best for spine and tendon pain. About 50-60% of patients get a 20% improvement (ACR20), and 30-40% get 50% improvement (ACR50).
- IL-17 inhibitors (secukinumab, ixekizumab): Better for skin and nails. Often preferred when psoriasis is severe.
- IL-12/23 inhibitors (ustekinumab): Good for both skin and joints.
- JAK inhibitors (tofacitinib): Oral pills that block inflammation signals. Used when biologics don’t work or aren’t an option.
Doctors now pick treatments based on what’s most active in your body. If your spine hurts more than your fingers, go with a TNF blocker. If your nails are shredded and your skin is covered, an IL-17 inhibitor might be better.
The Future Is Personalized
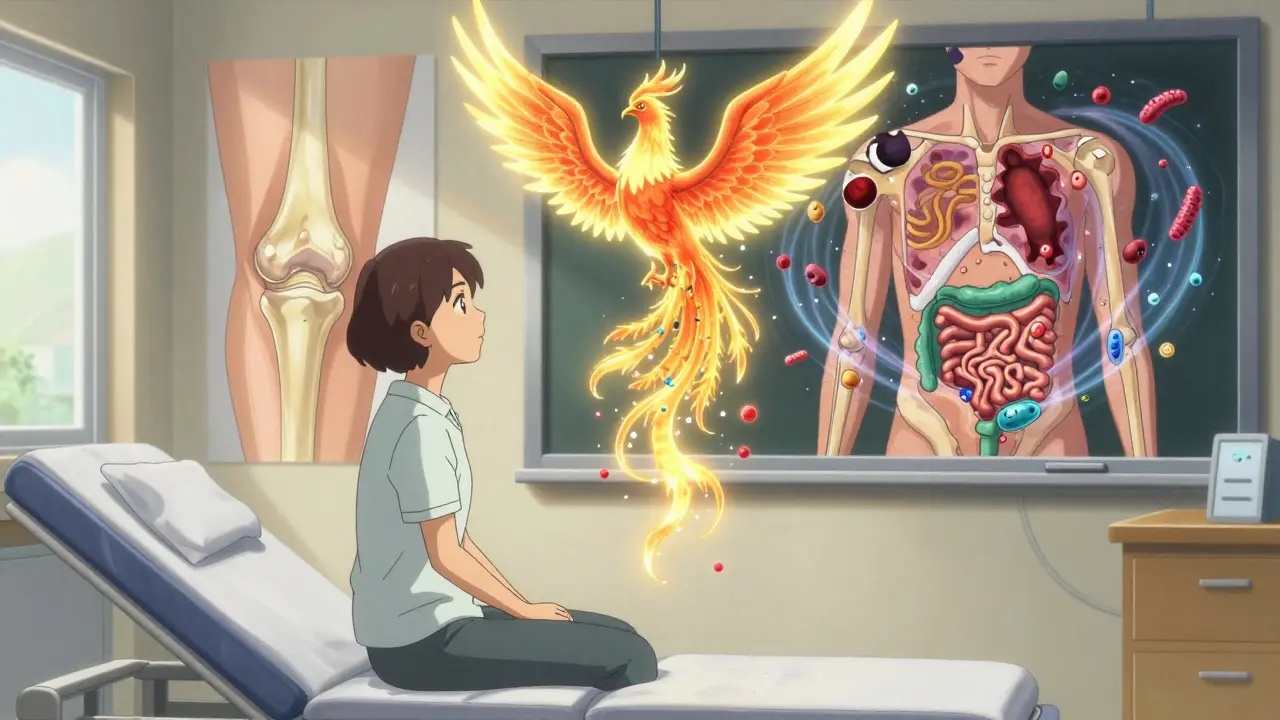
Research is moving fast. Scientists are finding new biomarkers-like MMP-3 and calprotectin in the blood-that might predict who will respond to which drug. Clinical trials are testing drugs like deucravacitinib (a TYK2 inhibitor) and bimekizumab (which blocks both IL-17A and IL-17F). One of the most exciting areas is the gut-skin-joint axis. Studies show people with PsA have different gut bacteria than healthy people. Could fixing your gut help calm your joints? Early trials are exploring probiotics and dietary changes as add-ons to medication. Advanced imaging is also helping. High-res ultrasound and MRI can now spot inflammation in tendons and joints before X-rays show damage. That means treatment can start earlier-before the joints are ruined. By 2027, experts predict 70% of PsA patients will be on biologics or targeted drugs within two years of diagnosis. That’s up from 40% today. Early treatment isn’t just about feeling better-it’s about keeping your body intact.What You Can Do Today
If you have psoriasis and notice new joint pain, stiffness, or swelling-don’t wait. See a rheumatologist. Don’t assume it’s just aging or overuse. The earlier you treat PsA, the better your chances of avoiding permanent damage. Lifestyle matters too. Losing weight cuts inflammation and makes medications work better. Quitting smoking helps. Regular movement-even walking-keeps joints flexible. And managing stress? That’s not just advice. It’s medicine. And don’t ignore your heart. Get your blood pressure, cholesterol, and blood sugar checked regularly. PsA isn’t just a skin and joint disease. It’s a cardiovascular risk factor too.It’s Not Just a Skin Condition
Psoriasis is visible. Psoriatic arthritis is not. But it’s just as real. And just as dangerous. The same immune system that makes your skin flake is quietly attacking your joints, your heart, and your future. You don’t have to live with pain. You don’t have to accept stiffness as normal. There are treatments that work. There are doctors who know how to help. And there’s hope-if you act before the damage becomes permanent.Can psoriasis turn into psoriatic arthritis?
Yes. About 30% of people with psoriasis develop psoriatic arthritis. In most cases, skin symptoms appear years before joint pain, but in 5-10% of cases, joint pain comes first. It’s not a guaranteed progression, but it’s common enough that anyone with psoriasis should watch for joint stiffness, swelling, or nail changes.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint swelling and pain, rheumatoid arthritis (RA) usually affects joints symmetrically and tests positive for rheumatoid factor. Psoriatic arthritis often affects joints unevenly, causes dactylitis (sausage fingers), enthesitis, and nail changes. People with PsA typically test negative for rheumatoid factor, which helps doctors tell them apart.
Can you have psoriatic arthritis without psoriasis?
Yes, but it’s rare. In 5-10% of cases, joint symptoms appear before any visible skin rash. These people often have a family history of psoriasis or develop skin patches later. Doctors still diagnose PsA using the CASPAR criteria, which includes past or family history of psoriasis-even if it’s not active at the time.
Does psoriatic arthritis show up on X-rays?
Early on, it might not. But in established cases, X-rays often show bone erosion, joint space narrowing, or the unique "pencil-in-cup" deformity where bone is both destroyed and rebuilt. Ultrasound and MRI are better for catching early inflammation before it shows on X-rays.
Can psoriatic arthritis be cured?
There’s no cure yet. But with the right treatment, most people can reach minimal disease activity-where symptoms are barely noticeable and joint damage stops progressing. Many stay in remission for years. Early, aggressive treatment is the key to avoiding long-term damage.
What’s the best diet for psoriatic arthritis?
No single diet cures PsA, but anti-inflammatory eating helps. Focus on omega-3s (fatty fish), colorful vegetables, whole grains, and nuts. Avoid processed foods, sugar, and excess alcohol, which worsen inflammation. Weight loss alone can reduce joint pain and improve medication response. Some people benefit from eliminating gluten or dairy, but that’s individual-talk to your doctor before making big changes.


8 Comments
January 11, 2026 McCarthy Halverson
Been dealing with this for 12 years. Skin cleared up with methotrexate but my knees never did. Started on adalimumab last year. Now I can walk without wincing. Don't wait like I did.
January 12, 2026 Michael Marchio
Everyone keeps talking about biologics like they're magic pills but nobody mentions the cost. A single shot of secukinumab runs over $20k a year. Insurance fights you every step. And don't get me started on the pre-auth forms. You spend more time on paperwork than living. This isn't medicine, it's a corporate grind disguised as healthcare.
January 14, 2026 Jake Kelly
My dad had psoriasis. I never thought I'd get it too. Then one morning my fingers felt like they were stuffed in gloves full of cement. Turned out to be PsA. Took me six months to find a rheumatologist who actually listened. I'm on ustekinumab now. Skin's better. Joints don't scream at dawn anymore. It's not perfect but it's progress.
January 14, 2026 Ashlee Montgomery
It's fascinating how the immune system doesn't distinguish between skin and joint tissue. The same molecular signals that cause flaking also trigger synovial inflammation. We treat the symptoms but rarely question why the body turns on itself. Is it genetics? Environment? Or something deeper we're missing? The gut microbiome connection might be the key we've overlooked for decades.
January 15, 2026 neeraj maor
They don't want you to know this but biologics are designed to keep you dependent. Big Pharma doesn't want a cure. They want lifelong customers. The real solution is detoxing your liver, cutting out gluten, and drinking alkaline water. I've seen people reverse it completely with just diet and fasting. The medical system won't tell you because it's not profitable.
January 15, 2026 Ritwik Bose
Thank you for sharing such a comprehensive and scientifically grounded overview 🙏 This information is invaluable for those navigating this journey. I have a cousin who was misdiagnosed for three years-this could have saved her so much pain. May we all advocate for earlier screening and compassionate care. 🌿
January 16, 2026 Paul Bear
It's critical to clarify that while NSAIDs and DMARDs provide symptomatic relief, they do not alter disease progression. Only biologics and JAK inhibitors target the IL-23/Th17 axis, which is the primary pathogenic pathway in PsA. The CASPAR criteria remain the gold standard for diagnosis because they integrate clinical, serological, and radiological findings-unlike the subjective, non-specific criteria used for RA. Failure to initiate targeted therapy within 12 months of symptom onset correlates strongly with radiographic progression (OR 3.4, p<0.01). Don't settle for palliation.
January 17, 2026 Jaqueline santos bau
I saw a guy at the grocery store with sausage fingers and I just knew. I went up to him and said 'You have PsA, don't you?' He looked at me like I was crazy. I told him about my cousin who lost her hands because she ignored it. He cried. I didn't mean to be pushy but someone has to say it. Nobody talks about this enough.
Write a comment