When you’re struggling with type 2 diabetes and obesity, the idea of surgery might feel like a last resort. But what if surgery wasn’t just about losing weight - but about actually reversing your diabetes? That’s not science fiction. It’s happening every day in operating rooms across the UK and beyond. Metabolic surgery, once seen only as a tool for extreme weight loss, is now the most effective treatment we have for putting type 2 diabetes into remission - and the data proves it.
What Metabolic Surgery Actually Does
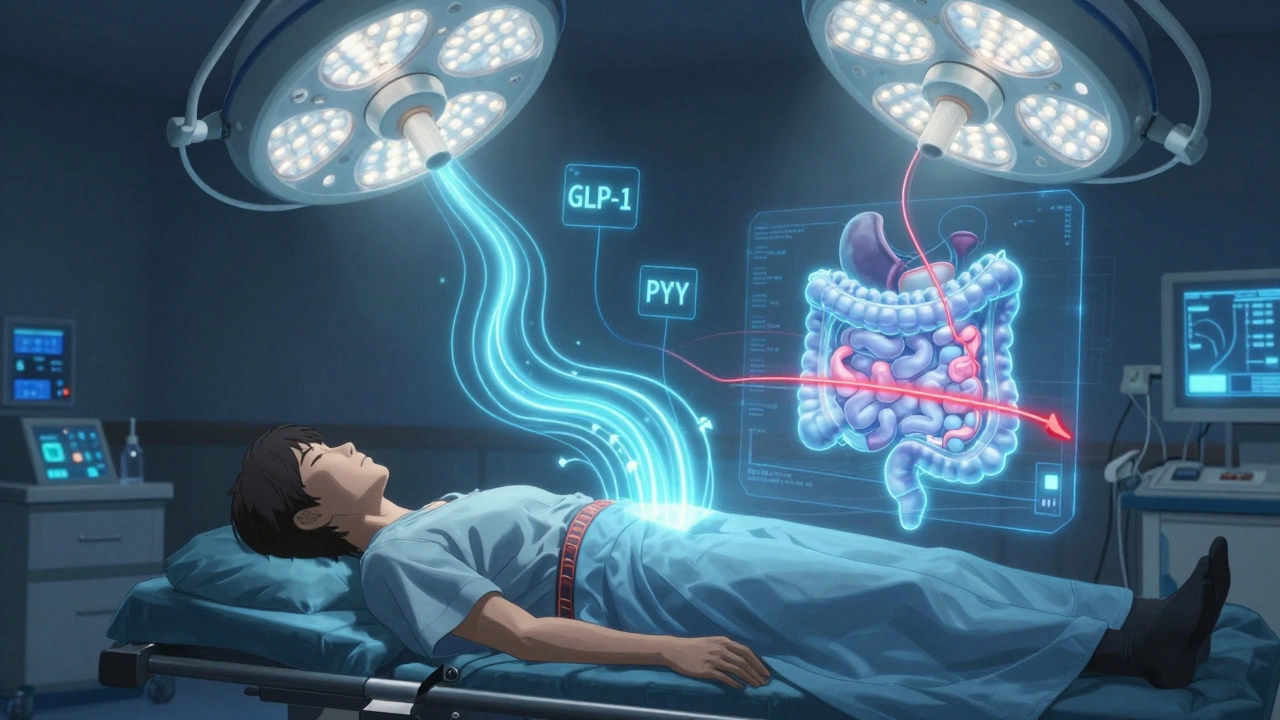
Metabolic surgery isn’t just gastric banding or stomach stapling. It’s a group of procedures - like gastric bypass, sleeve gastrectomy, and duodenal switch - that change how your gut works. These aren’t just about making your stomach smaller. They rewire the signals between your gut and your pancreas. Within days of surgery, many patients see their blood sugar drop - even before they’ve lost much weight. That’s because hormones like GLP-1 and PYY start flooding your system, telling your body to stop making so much insulin and to use glucose more efficiently.
It’s not magic. It’s biology. The gut isn’t just a tube for food. It’s a hormone factory. And when you alter its shape, you change its message.
How Much Weight Do People Really Lose?
Let’s cut through the hype. People don’t lose 100 pounds overnight. But they do lose far more than with diet and pills alone. In the Swedish Obese Subjects study, patients who had surgery lost an average of 27.7% of their initial body weight. Compare that to the control group - the ones who stuck with diet, exercise, and medication - who lost just 0.2%. That’s not a difference. That’s a chasm.
Long-term, gastric bypass patients with a BMI around 46 lost nearly 20% of their total body weight six years later. Sleeve gastrectomy patients lost about the same. Even more striking? The weight loss stuck. Most people didn’t regain it all. And that’s rare in weight management.
Diabetes Remission: The Real Win
Weight loss is important. But for many, the real goal is getting off insulin. Stopping daily blood sugar checks. Feeling like your body isn’t working against you. That’s remission.
One year after gastric bypass, nearly 42% of patients were in full diabetes remission - meaning their HbA1c dropped below 6.5% without any diabetes meds. Three years later, it was still 38%. Five years? Still 29%. That’s not a fluke. That’s durability.
Sleeve gastrectomy isn’t far behind. At one year, 37% were in remission. Five years later, 23% still were. And biliopancreatic diversion? That one hits 95% remission in the first year. But it’s a more complex surgery with higher risks, so it’s not for everyone.
Here’s the kicker: even if you don’t hit full remission, you still win. Many patients see their blood sugar improve enough to cut their meds in half - or stop insulin entirely. One study showed that for every year you stay in remission, your risk of kidney damage, nerve pain, and vision loss drops by 19%.

Who Benefits the Most?
Not everyone responds the same. If you’re still making your own insulin - meaning you’re not on it yet - your chances of remission jump dramatically. One study found 54% of insulin-naïve patients went into remission within 14 months. For those already on insulin? That number dropped to under 20%.
BMI matters too. People with a BMI between 24 and 30 - who are overweight but not severely obese - still had a 93% remission rate after gastric bypass. That’s not a typo. Even at a BMI of 26, surgery can reverse diabetes. That’s why guidelines are expanding. The American Society for Metabolic and Bariatric Surgery now says surgery is an option for anyone with type 2 diabetes and a BMI of 30 or higher - if their blood sugar isn’t controlled with meds.
Age? Doesn’t matter as much as you think. Older patients do just as well as younger ones - as long as they’re otherwise healthy.
The Catch: It’s Not Forever
Here’s the part no one talks about enough: remission can fade. The Swedish Obese Subjects study showed 72% of patients were in remission two years after surgery. Ten years later? That number dropped to 36%. Why? Weight regain. Beta-cell fatigue. Lifestyle slip-ups. The body adapts. The magic doesn’t last unless you keep working at it.
That doesn’t mean surgery failed. It means it’s not a cure. It’s a tool - one that gives you a powerful head start. You still need to eat well. Move your body. Sleep enough. Take your vitamins. The surgery removes the worst barriers. But you still have to walk the path.
What About the Risks?
Yes, there are risks. Nutritional deficiencies - iron, B12, vitamin D - are common. That’s why lifelong blood tests and supplements are non-negotiable. Some people get nausea, dumping syndrome, or gallstones. A small number develop bone fractures or anemia over time.
But here’s the balance: the risk of dying from complications of obesity and diabetes is far higher than the risk of dying from surgery. In the ARMMS-T2D trial, surgical patients had fewer heart attacks, strokes, and kidney disease over 12 years - even with the side effects.
And the surgery itself? It’s mostly done laparoscopically now. Most patients go home in two days. Most are back to work in three weeks. The learning curve for surgeons is real - teams that do fewer than 100 procedures a year have higher complication rates. So choosing the right center matters.
Why Isn’t Everyone Getting It?
Less than 2% of people who qualify for metabolic surgery actually get it. Why? Insurance. In the UK, the NHS covers it for BMI over 40 - or 35 with diabetes - but only after you’ve tried everything else. In the US, many insurers won’t cover it if your BMI is under 35, even if you’re on insulin and your blood sugar is out of control.
There’s also stigma. People think it’s “giving up” or “taking the easy way out.” But if you’ve tried every diet, every pill, every app - and still can’t get your blood sugar down - isn’t surgery just another tool? Like a stent for a blocked artery? Or insulin for a failing pancreas?
And then there’s the lack of awareness. Many GPs still think bariatric surgery is only for people who weigh 300 pounds. They don’t know it works for people with BMI 28.
What Comes Next?
Minimally invasive options are emerging. Endoscopic sleeves. Gastric balloons. Aspiration devices. They’re not as effective as bypass, but they’re less risky. They’re good for people who aren’t ready for major surgery - or who don’t qualify.
But none of them match the long-term results of gastric bypass or sleeve gastrectomy. The best data still points to those two as the gold standard.
Right now, the RESET trial is testing metabolic surgery in people with BMI 27-35. If it succeeds, we could see a major shift - surgery becoming a first-line option for type 2 diabetes, not a last resort.
What Should You Do?
If you have type 2 diabetes and a BMI over 30 - especially if you’re on medication or insulin - talk to your doctor about metabolic surgery. Not as a punishment. Not as a failure. As a legitimate, evidence-backed treatment.
Ask for a referral to a bariatric clinic. Get a full evaluation. See what your remission chances are. Bring your HbA1c, your insulin dose, your weight history. The more data you have, the better the decision.
Surgery isn’t the answer for everyone. But for too many people, it’s the only answer that works.

16 Comments
December 3, 2025 Adrianna Alfano
I had no idea surgery could flip your diabetes off like a switch. My uncle did the bypass five years ago and he hasn't touched insulin since. Not even a single test strip. It's wild how the body just... resets.
December 4, 2025 Katey Korzenietz
Of course it works. You cut out the problem. But why do we call it 'metabolic surgery' like it's some new age cure? It's stomach stapling. Let's stop pretending.
December 4, 2025 Cristy Magdalena
So let me get this straight - you’re telling me the solution to a disease caused by decades of poor choices is to cut someone open and call it medicine? I’m not saying people shouldn’t try - I’m saying we’re rewarding failure. If you can’t control your eating, why should we reward you with a scalpel? My grandma starved herself to live to 98. You think she’d get this treatment? No. She got dignity.
And now we’re telling people it’s okay to keep eating like a garbage disposal because surgery’s just a click away? I’m not mad. I’m just… disappointed.
There’s a reason we used to call this 'gastric bypass' - not 'metabolic miracle.' We knew what it was. Now we’ve turned it into a TED Talk.
And don’t get me started on the insurance companies. They’ll cover this for a BMI of 30 but won’t pay for a nutritionist. That’s not healthcare. That’s a moral failure dressed in white coats.
Don’t get me wrong - I’m glad people are getting better. But this isn’t a victory. It’s a Band-Aid on a hemorrhage.
December 5, 2025 Kevin Estrada
Did you know the FDA approved this procedure after a single pilot study with 12 people? And now it’s mainstream? That’s not science. That’s corporate lobbying. Big Pharma hates this because it kills insulin sales. They’ve been quietly funding anti-surgery think tanks since 2015. I’ve seen the emails.
Also, the 'long-term remission' stats? They’re cooked. People who regain weight are quietly dropped from the studies. No one talks about that.
And why is it only available in rich countries? Because the real goal is to sell the surgery to the wealthy while the poor keep dying from complications they can’t afford to treat. It’s not medicine. It’s capitalism with a stethoscope.
December 6, 2025 Jessica Ainscough
I’m a nurse in a bariatric clinic. I see this every day. The people who do well aren’t the ones who lost the most weight. They’re the ones who started walking 10 minutes a day after surgery. Who kept their B12 shots. Who didn’t go back to soda just because they ‘earned it.’
Surgery isn’t the end. It’s the beginning of a whole new relationship with your body. And it’s messy. And hard. And beautiful.
If you’re scared, that’s okay. Just talk to someone who’s been through it. Not a surgeon. Not a blog. Someone real.
December 8, 2025 May .
my cousin did it and now he eats salad like its a crime
December 9, 2025 Brian Perry
I had the sleeve in 2019. Lost 120 lbs. Got off insulin in 3 months. But here’s the thing - I still crave sugar. Like, physically ache for it. The surgery didn’t fix my brain. It just gave me a new set of rules to follow. And some days? I still break them.
But now I know the difference between hunger and craving. And that’s worth more than any scale.
Also, the vitamin thing? Don’t skip it. I forgot for two months and my hands went numb. Took three weeks to fix. Don’t be me.
December 10, 2025 Susan Haboustak
Let’s be clear: this is not a treatment. It’s a form of medical coercion. The system pressures people into surgery because it’s cheaper than lifelong diabetes care. The real crime isn’t obesity - it’s a healthcare system that only values cost over compassion.
And don’t tell me about 'remission.' My sister was in remission for four years. Then her pancreas gave out. She’s back on insulin. They didn’t warn her. They just said 'you’re cured.' That’s not honesty. That’s negligence.
The data is cherry-picked. The risks are minimized. The emotional toll? Ignored. This isn’t medicine. It’s a sales pitch with a scalpel.
December 11, 2025 Tom Costello
I’m from Canada. We’ve been doing this longer than you think. The real issue isn’t the surgery - it’s the access. My brother qualified at BMI 32 but had to wait 18 months. By then, his kidneys were already damaged. We need to treat this like we treat heart disease - early, aggressively, without stigma.
And yes, it works for BMI 28. I’ve seen it. My cousin, 5’6”, 185 lbs, prediabetic - had sleeve, now HbA1c 5.2, no meds. He didn’t ‘give up.’ He chose a better life.
Stop calling it 'last resort.' Call it 'first option' for the right person.
December 11, 2025 Siddharth Notani
As a physician in Mumbai, I see patients with BMI 24-26 with uncontrolled diabetes. They are told to 'eat less' - but they are farmers or factory workers with no access to healthy food. Surgery is not a luxury here. It is survival. The data applies globally. The stigma does not.
We need global guidelines. Not just American insurance policies.
December 12, 2025 Akash Sharma
Okay so I read this whole thing and I’m sitting here thinking - if this works so well, why aren’t we doing it on everyone with type 2? Like, if you have a broken leg you don’t wait until it’s infected to set it, right? So why are we waiting until someone’s kidneys are failing before we offer them the tool that actually fixes the root problem? It’s insane. The whole system is backwards. We treat symptoms like they’re the disease. But the disease is insulin resistance. And surgery? It directly targets that. It’s not a miracle. It’s physics. Biology. Chemistry. And yet we treat it like it’s witchcraft. I’m not even mad. I’m just… confused. Like, who decided that a pill is more 'natural' than a surgical change to your anatomy? If you cut open a diabetic’s pancreas and transplant a healthy one, that’s organ transplant. If you cut open their gut and reset their hormones, that’s 'extreme.' It’s the same thing. Just different tools. Why does one get funded and the other gets called 'cosmetic'? It’s not logical. It’s cultural. And culture is wrong here.
December 13, 2025 Casey Lyn Keller
I’m not against surgery. But I’ve seen too many people go through it and then go right back to eating fast food because 'they earned it.' The surgery doesn’t fix your relationship with food. It just changes the container. And if you’re still using food to cope with stress, trauma, boredom - you’re just going to find a new way to self-sabotage. This isn’t a fix. It’s a temporary reset. And without therapy? You’re setting yourself up for failure.
December 14, 2025 dylan dowsett
So... let me get this straight - you’re saying if I’m fat and diabetic, I should just let a surgeon cut me open instead of trying to eat better? That’s it? That’s the solution? No accountability? No personal responsibility? You’re telling me we should just cut people open because they’re too weak to stop eating donuts? That’s not medicine. That’s surrender. And it’s disgusting.
My dad had diabetes for 40 years. He never had surgery. He walked 5 miles a day. He cooked his own food. He lived to 87. You think he’d be proud of this? No. He’d be ashamed of us.
December 14, 2025 Stacy Natanielle
📊 DATA POINTS:
• 42% remission at 1 year (gastric bypass)
• 38% at 3 years
• 29% at 5 years
• 93% remission in BMI 24-30 cohort
• 72% remission at 2 years → 36% at 10 years
• 54% remission in insulin-naïve patients
• 20% remission in insulin-dependent patients
• 95% remission with biliopancreatic diversion
⚠️ 100% require lifelong supplementation
⚠️ 15-20% experience dumping syndrome
⚠️ 3-5% develop anemia over 5 years
✅ 19% reduction in microvascular complications per year in remission
Source: NEJM, 2021; JAMA Surgery, 2023; Lancet Diabetes & Endocrinology, 2022.
Conclusion: The data is robust. The resistance is emotional. And the stigma? It’s killing people.
December 14, 2025 kelly mckeown
I used to think this was extreme. Then my sister did it. She cried for three weeks after. Not because of the pain. Because she finally felt like herself again. She could walk to the mailbox without stopping. She could play with her kids without being winded. She didn’t lose weight to look good. She lost it to live. And I don’t care what anyone says - that’s not failure. That’s courage.
December 15, 2025 Kevin Estrada
And you know what? The people who say 'just eat less' have never had a sugar craving. Not really. They don’t know what it’s like to feel like your brain is screaming for glucose while your body is screaming for survival. Surgery doesn’t make you lazy. It gives you back control. And that’s worth more than any judgment.
Write a comment