It’s not just about running out of medicine. The real crisis in hospitals and clinics right now is that there aren’t enough people to give care-even when the drugs are on the shelf. By late 2024, over 42 U.S. states were already facing serious nursing shortages, and the numbers keep climbing. Hospitals are closing beds. Emergency rooms are seeing 72-hour waits. Clinics in rural areas are shutting down entire services because they can’t find staff. This isn’t a future problem. It’s happening today, and patients are paying the price.
Why There Aren’t Enough Nurses and Doctors
The root of this problem goes back years, but the pandemic turned a slow leak into a flood. More than half of all nurses in the U.S. are over 50, and nearly one-third will retire in the next 10 to 15 years. At the same time, nursing schools can’t train enough new nurses because there aren’t enough faculty to teach them. The American Association of Colleges of Nursing reports that over 2,300 qualified applicants were turned away from nursing programs in 2023-just because there weren’t enough instructors. Doctors aren’t immune. The Association of American Medical Colleges predicts a shortage of 86,000 physicians by 2036. Primary care is hit hardest. Rural clinics, which already struggle to attract talent, now operate at just 58% staffing levels-far below the 79% seen in urban clinics. And it’s not just numbers. The people who stay are burned out. In 2025, 63% of nurses said they were thinking about leaving the profession. The main reason? Unsafe patient ratios.What Happens When Staffing Drops Below Critical Levels
When a hospital has more patients than nurses, things fall apart fast. Research from JAMA shows that when nurse-to-patient ratios go above 1:4, patient death rates jump by 7%. That’s not a small uptick. That’s lives lost because one nurse is trying to care for five people at once. Emergency departments are drowning. The American College of Emergency Physicians found that understaffed ERs now have 22% longer wait times than they did in 2022. Patients with chest pain, strokes, or severe infections wait hours-sometimes days-for basic care. In rural Nevada, patients reported waiting up to 72 hours in the ER. That’s not an outlier. It’s becoming the norm. In long-term care facilities, the shortage is even worse. These places now have 28% fewer nurses than they did before the pandemic. Residents are going without baths, medications are delayed, and pressure sores go untreated. Families are noticing. Complaints on Healthgrades about long waits and poor care rose 27% since 2022.The Ripple Effect: From ERs to Operating Rooms
It’s not just nurses. Surgeons can’t operate if there’s no anesthesiologist. Radiologists can’t read scans if the techs aren’t there. Cardiac care units are turning away patients because they can’t staff the monitors. Operating rooms are canceling surgeries-sometimes on the day of-because nurses and techs call out sick or are already stretched too thin. The American Hospital Association found that 12% of hospital beds are closed every week just because there’s no one to staff them. Mercy Health’s CEO reported losing $4.2 million a month in revenue because of these closures. That’s not just a financial hit. It’s a health crisis. People with chronic conditions can’t get routine care. Cancer patients miss chemo appointments. Diabetics can’t get their insulin adjusted. And then there’s behavioral health. The Department of Health and Human Services says there’s a nationwide deficit in mental health providers. People in crisis wait days in ERs because there’s no bed, no therapist, no psychiatrist. Some are discharged without follow-up because the system can’t handle them. Suicide rates are rising in communities where mental health services have vanished.
Temporary Fixes That Make Things Worse
Hospitals are scrambling. Many are turning to travel nurses-contract workers who move from hospital to hospital. In 2023, travel nurses filled 12% of hospital positions. But they cost three times more than permanent staff. In New York, travel nurses are earning $185 an hour. Meanwhile, the nurse who’s been working there for 15 years makes $65. Resentment is building. Morale is crashing. Some hospitals are forcing staff to work mandatory overtime-twice a week or more. That’s not sustainable. Nurses are exhausted. One ICU nurse on Reddit wrote about working 16-hour shifts with three patients and nearly making two medication errors last month. That’s not negligence. That’s burnout. Telehealth was supposed to help. But setting up remote triage systems costs $2.3 million per health system-and even then, only 19% fewer ER visits. And not every patient can use it. Elderly patients, non-English speakers, and those without smartphones are left behind.Why Solutions Keep Failing
The problem isn’t that we don’t know what to do. We do. We need more nursing scholarships. We need better pay. We need state licensing to be easier so nurses can move across state lines. We need AI tools to handle paperwork so nurses can focus on patients. But here’s the catch: most hospitals don’t have the money. Small clinics can’t afford $4.7 million to redesign care teams like Mayo Clinic did. And federal funding? The American Medical Association says the government spends $247 million a year on nursing education-when it needs $1.2 billion just to keep up. Even when programs are launched, they move too slowly. Training a nurse to use new AI documentation tools takes 8.7 weeks and 32 hours of class time. State licensing delays for telehealth nurses average 112 days. By the time the system adapts, the crisis has deepened.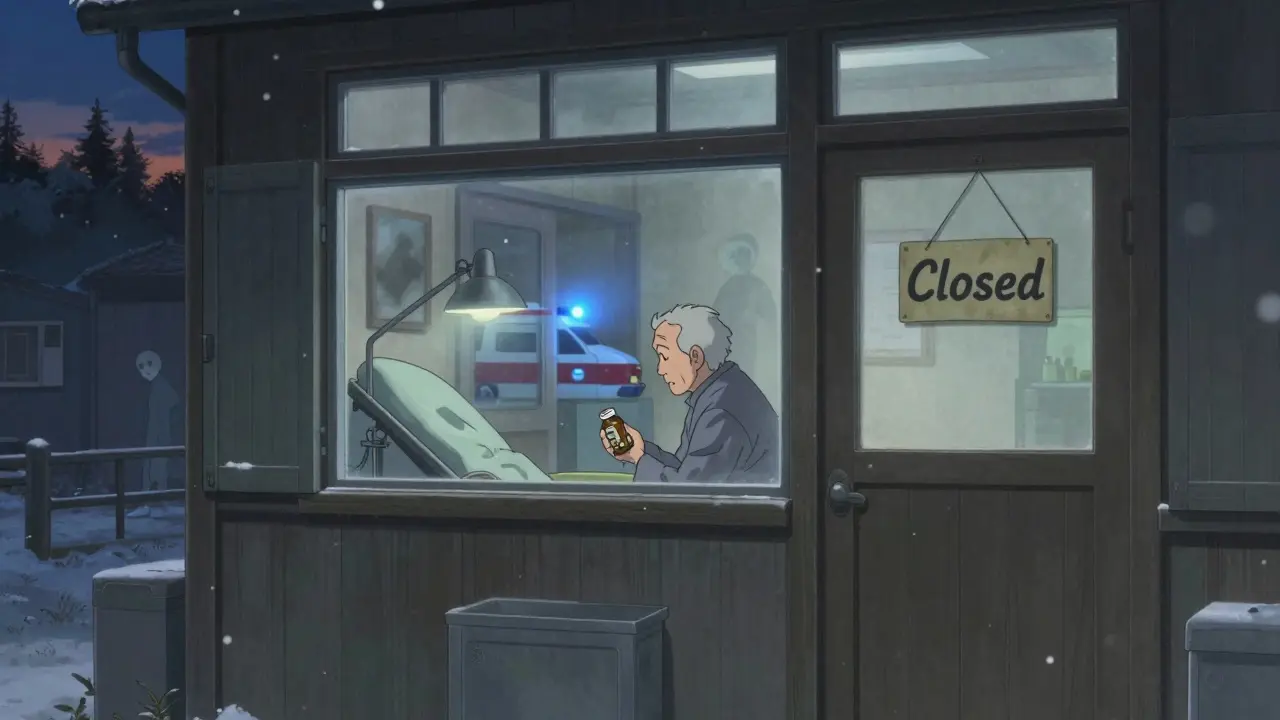
Who’s Getting Left Behind
This isn’t an equal crisis. It’s worse in rural areas, where hospitals are already underfunded. Rural facilities have 37% higher vacancy rates than urban ones. In places like West Virginia or eastern Kentucky, the nearest ER might be 60 miles away. When the clinic closes because the nurse quits, that’s it. Older adults are hit hardest. With 55 million Americans over 65 today-and 82 million expected by 2050-the demand for care is skyrocketing. But the workforce shrinking. By 2030, there will be only 2.9 working-age people for every senior. Right now, it’s 4:1. That math doesn’t work. Minority communities suffer too. Black and Hispanic patients are more likely to live in areas with fewer providers. When clinics close, they’re the ones who lose access first.What’s Actually Changing
Some progress is happening, but it’s slow. California passed laws requiring 1:5 nurse-to-patient ratios in medical-surgical units. Massachusetts cut its nursing shortage to 8% below the national average by offering loan forgiveness. The Biden administration just allocated $500 million for nursing education-but experts say that’s only 18% of what’s needed. The American Hospital Association is launching a new initiative in June 2025 to train 50,000 new healthcare workers. But it’s a drop in the ocean. The global shortage is projected to hit 15 million workers by 2027. We’re talking about millions of missing caregivers. The only real hope is combining better pay, better working conditions, and smarter use of technology. AI can help with scheduling. Remote monitoring can reduce hospital readmissions. But none of it works without people to manage it.The Bottom Line
This isn’t a temporary glitch. It’s a structural collapse. Hospitals and clinics aren’t just understaffed-they’re broken. And until we treat healthcare workers as the critical resource they are-not as replaceable cogs-we’ll keep seeing the same outcomes: longer waits, more errors, and preventable deaths. The drugs are there. The machines are there. But the hands to hold the patient, the eyes to read the monitor, the voice to explain what’s happening-those are vanishing. And no algorithm can replace that.Why are hospitals closing beds due to staffing shortages?
Hospitals close beds because they don’t have enough nurses, doctors, or support staff to safely care for patients. Even if a bed is available, if there’s no one to monitor vital signs, give medications, or respond to emergencies, keeping it open puts patients at risk. In 2024, some hospitals closed 12 beds per week just to avoid unsafe conditions.
Are travel nurses solving the staffing crisis?
They’re a temporary fix, not a solution. Travel nurses filled 12% of hospital positions in 2023, but they cost 34% more than permanent staff. This drives up hospital expenses and creates resentment among full-time staff who earn much less. Many travel nurses move on after a few months, leaving hospitals right back where they started.
How do staffing shortages affect patient safety?
When nurses are stretched too thin, mistakes happen. Studies show that when nurse-to-patient ratios exceed 1:4, patient death rates rise by 7%. Medication errors, missed signs of deterioration, and delayed responses to emergencies become more common. In one case, an ICU nurse reported two near-miss errors in one month because she was caring for three patients at once.
Why can’t we just hire more nurses?
There aren’t enough nursing schools with the faculty to train them. In 2023, over 2,300 qualified applicants were turned away from nursing programs because there weren’t enough instructors. Even if we opened more schools, it takes four years to train a registered nurse. We’re not building the pipeline fast enough.
Is telehealth helping with the shortage?
It helps in some ways-like reducing unnecessary ER visits by 19% in pilot programs-but it’s not a cure-all. Many patients, especially older adults and those in rural areas, can’t use it. Setting up telehealth systems costs millions, and many clinics can’t afford it. Plus, 68% of hospitals still struggle with electronic health record systems that don’t talk to each other.
What’s the long-term outlook for healthcare staffing?
Without major changes, shortages will get worse. The U.S. nursing shortage could last until 2035. By 2030, 42 states will still be short on nurses. The global shortage of healthcare workers is expected to peak at 15 million by 2027. Technology and policy changes could offset 30-40% of the gap-but only if we invest billions now.


9 Comments
December 16, 2025 Donna Packard
It breaks my heart to see nurses working 16-hour shifts just to keep people alive. I know they’re exhausted, but I also know they’re the reason my mom made it through chemo. We need to treat them like heroes, not disposable workers.
They’re not just filling out charts-they’re holding hands, explaining diagnoses, staying up all night when no one else will. That’s not a job. That’s love in scrubs.
December 16, 2025 Patrick A. Ck. Trip
While i agree with the core issues raised here, the solutins proposed seem overly reliant on federal funding without addressing systemic inefficiencies in administrative burden. The paperwork load on nurses is obscene, and ai tools could alleviate this-if properly implemented with user-centered design.
unfortunatly, most hospitals still use ehrs from the early 2000s that dont talk to each other, making even simple tasks a nightmare.
December 18, 2025 Sam Clark
As someone who has worked in hospital administration for over two decades, I can confirm that the staffing crisis is not simply a matter of wages or recruitment-it is a failure of institutional prioritization.
Hospitals have spent the last 15 years optimizing for profit margins rather than patient outcomes. When you cut nursing positions to boost quarterly earnings, you don’t just reduce costs-you erode the very foundation of care.
It’s not about spending more money. It’s about spending it differently. Invest in retention before you invest in recruitment.
December 19, 2025 Jessica Salgado
I worked in a rural ER for five years. I’ve seen patients wait 72 hours because there was no one to admit them. I’ve watched a diabetic go into ketoacidosis because the only nurse on shift was dealing with three cardiac arrests.
It’s not just burnout. It’s betrayal. We were told this was a noble calling. But no one told us we’d be asked to choose between our sanity and someone’s life every single shift.
And now they want us to be grateful for a $5k signing bonus? Please.
I left last year. I’m a barista now. At least when I mess up a latte, no one dies.
December 20, 2025 Kaylee Esdale
the machines are fancy but the hands are gone
no app can hold your hand when you’re scared
no robot can tell your grandma its gonna be okay
we forgot that care is human
December 21, 2025 BETH VON KAUFFMANN
Let’s be clear: the nursing shortage is a supply-side failure exacerbated by unionized wage inflation and regulatory capture by nursing schools that restrict enrollment to maintain artificial scarcity.
AI-driven triage systems, expanded scope of practice for LPNs, and accelerated certification tracks for paramedics could resolve 60% of the crisis without increasing public expenditure.
Instead, we’re throwing $500M at a problem that requires structural deregulation, not more subsidies.
December 22, 2025 Meghan O'Shaughnessy
Coming from India, I’ve seen how community health workers fill gaps where formal systems fail. In rural India, ASHA workers-barely paid, no degrees-deliver meds, educate families, and monitor chronic illness.
What if we trained and paid community members in West Virginia or Kentucky to do the same? Not to replace nurses, but to support them?
It’s not about replacing the system. It’s about expanding it with what already exists.
December 23, 2025 Philippa Skiadopoulou
UK NHS has faced similar pressures for years. The solution isn’t just pay-it’s workload redistribution.
We now have nurse practitioners managing 70% of primary care cases that used to go to GPs. It reduces pressure, improves access, and retains staff.
Why aren’t we doing this here? Because the medical establishment resists delegation. Not because it doesn’t work.
December 23, 2025 Pawan Chaudhary
My sister is a nurse in Chicago. She told me last week that her hospital just hired 12 travel nurses at $180/hour. Meanwhile, her colleague who’s been there 18 years makes $68/hour.
She said, 'We’re not mad they’re paid more. We’re mad that we’re not valued enough to be paid that much too.'
That’s the real problem.
Write a comment