Diabetes Remission: What It Really Means and How It Happens
When people talk about diabetes remission, a state where blood sugar returns to normal without medication. It's not a cure, but it's not a myth either—this is what happens when your body regains control over insulin and glucose after years of relying on pills or injections. For many with type 2 diabetes, remission isn’t something that happens to lucky few—it’s something you can earn through consistent, realistic changes.
It’s not about starving yourself or becoming a gym addict. It’s about weight loss, especially around the liver and pancreas. Studies show that losing just 5–10% of your body weight can reset how your body handles sugar. That’s not magic—it’s biology. When fat builds up in those organs, they stop responding properly to insulin. Take that fat off, and the organs start working again. You don’t need to lose 50 pounds. Sometimes, losing 15–20 pounds is enough to get off medication for good. This isn’t theoretical. Real people, with real jobs and real lives, have done it.
blood sugar control, the daily management of glucose levels through food, activity, and sometimes drugs. Remission doesn’t mean you stop paying attention. It means you’ve moved from reacting to sugar spikes to preventing them. That’s where diet becomes your most powerful tool—not because you have to avoid carbs forever, but because you learn to eat them in ways your body can handle. Think less white bread, more beans and vegetables. Less sugary drinks, more water. And timing matters. Eating the same meals at the same times every day helps your body predict and manage insulin better.
lifestyle changes, daily habits that affect long-term health, including diet, movement, and sleep. These aren’t just buzzwords. Walking 30 minutes a day, sleeping 7 hours, and reducing stress aren’t optional extras—they’re the foundation. One study found that people who combined weight loss with daily walking were over twice as likely to reach remission than those who only changed their diet. And sleep? Poor sleep raises cortisol, which raises blood sugar. Fix that, and you fix half the battle.
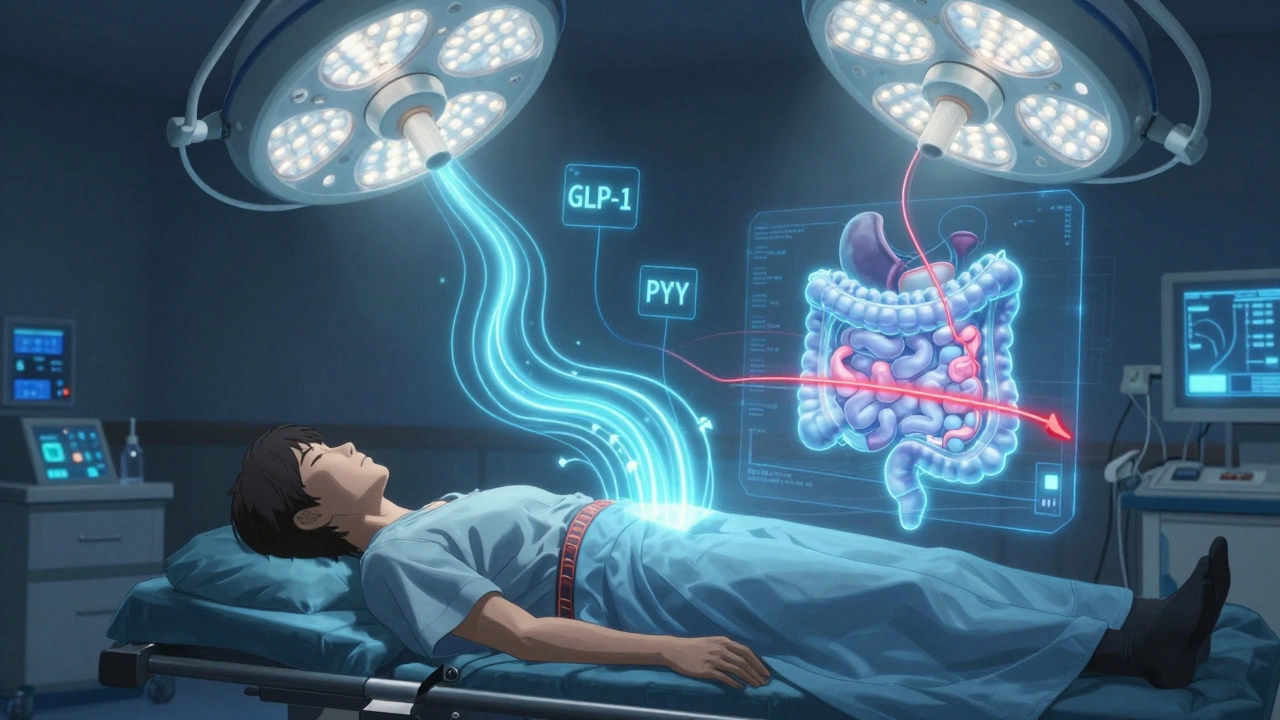
And then there’s medication reduction, the process of lowering or stopping diabetes drugs under medical supervision. Some people stop metformin. Others stop insulin. But you don’t just quit cold turkey. Remission is confirmed through lab tests—not how you feel. Your doctor checks your HbA1c, fasting glucose, and sometimes even insulin levels to make sure your body can handle it without help. That’s why you can’t do this alone. You need guidance, monitoring, and a plan.
What you’ll find below aren’t just articles about diabetes. These are real stories and science-backed facts about how people got off meds, what worked, what didn’t, and how to avoid the traps that send people right back to square one. Some of these posts talk about how generic drugs interact with diet. Others show how sleep aids or painkillers can mess with your blood sugar. You’ll see how switching medications can affect your progress. And you’ll learn what to watch for when your body starts to heal.